Weight Management: Losing Weight Is Reducing "Inflammation" — The Scientific Link Between Obesity and Psoriasis
。
If you are a psoriasis patient and overweight, take this seriously — obesity is not only an appearance concern but also an important driver of disease activity.
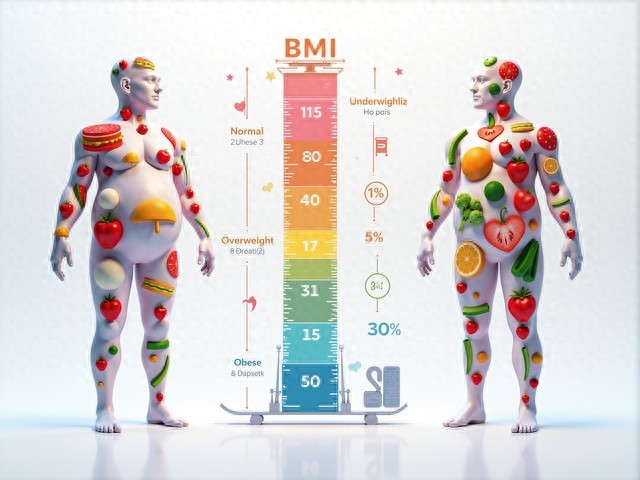
Numerous epidemiological studies have confirmed that the prevalence of obesity in patients with psoriasis is significantly higher than in the general population; for each 1-unit increase in BMI, the risk of disease increases by 9%; and among patients with severe psoriasis, nearly half have concomitant obesity. The mechanism is that adipose tissue (especially visceral fat) is not an inert energy reservoir but an active endocrine “factory,” continuously secreting proinflammatory factors such as leptin, resistin, TNF-α, and IL-6, creating a state of chronic low-grade inflammation that directly exacerbates skin and joint lesions.
More worrisome, obesity also reduces treatment response. Studies show that obese patients treated with methotrexate or biologics have a significantly lower probability of achieving PASI 75 (75% improvement in skin lesions) compared with individuals of normal weight.
Therefore, weight loss should be considered part of psoriasis management. The goal is not to become extremely thin, but a healthy weight loss of 5%–10% — an amount that has been shown to significantly improve lesion area and severity. I recommend a “gentle and sustainable” strategy:
Diet: Adopt a Mediterranean dietary pattern, control total calorie intake, and increase dietary fiber and high-quality protein;
Exercise: Combine aerobic (brisk walking, swimming) and resistance training (resistance bands, bodyweight exercises), 150 minutes per week;
Behavioral interventions: keep a food diary, set small goals, seek family support.
Weight loss may be slow, but each step is "extinguishing" the inflammatory fire in the body. When you start managing your weight, you are actively treating psoriasis.