Two Dietary Habits That Most Harm the Pancreas in Diabetics, Four Methods to Protect the Pancreas, and How to Test Pancreatic Function
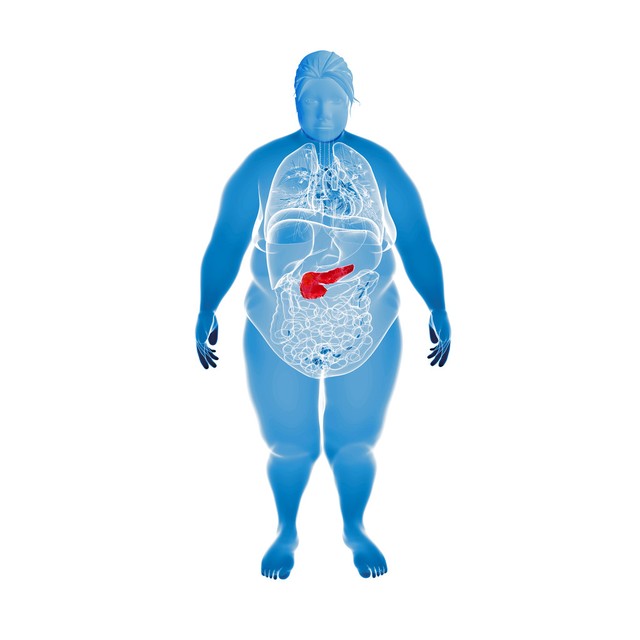
From the moment of being diagnosed with diabetes, patients often face significant lifestyle adjustments and severe challenges in self-management. Diabetes, this chronic disease, not only affects the patient's daily life but also causes irreversible damage to the pancreatic islet function. Studies indicate that at the time of diagnosis, a patient's islet function may already be reduced by nearly half, and this damage continues to worsen at an annual rate of 5%. Faced with this reality, we must deeply recognize that protecting islet function and slowing the progression of diabetes have become crucial issues that every person with diabetes must prioritize.

Excessive Oil Intake for People with Diabetes: A Killer of Islets
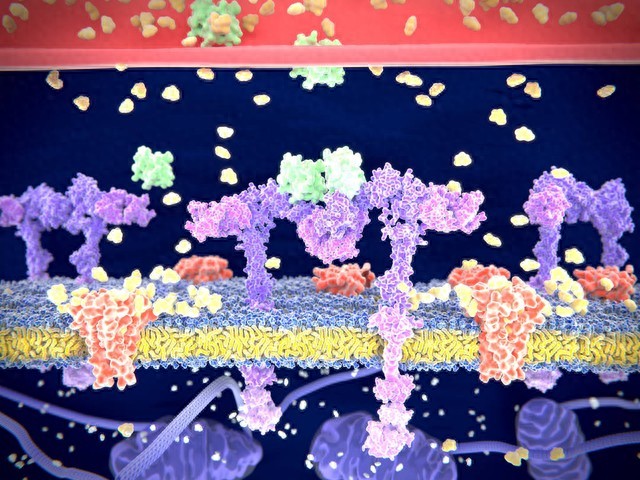
In daily diets, fat intake is often overlooked, yet it is an "invisible killer" that damages islet function. Excessive fat intake, particularly from using too much oil in stir-frying, frequent consumption of fried foods, or high-fat meats, can overwhelm the body. These excess fats are broken down into free fatty acids, which, like "unwelcome guests," travel to pancreatic beta cells, causing direct damage and impairing normal insulin secretion.
More seriously, a high-fat diet is often accompanied by excess energy, easily leading to weight gain. Obesity is one of the significant triggers for diabetes. It not only increases the burden on pancreatic beta cells but also exacerbates insulin resistance by affecting the sensitivity of insulin receptors. Therefore, for people with diabetes, controlling fat intake and choosing low-fat, high-protein foods such as fish, shrimp, poultry, and lean meat is the first step in protecting islet function.
Excessive Consumption of Liquid Foods for People with Diabetes: Increasing the Burden on Islets
Besides fats, liquid foods like congee are also a "sweet trap" that people with diabetes need to be wary of. During the cooking process of rice or flour, starch undergoes gelatinization, making congee extremely easy to digest and absorb. After entering the body, blood sugar rises rapidly, akin to "drinking congee like sugar water." This rapid rise in blood sugar, followed by a swift drop, leads to significant blood sugar fluctuations, frequently stimulating pancreatic beta cells and accelerating their damage.
Therefore, people with diabetes should try to avoid congee in their daily diet, opting instead for healthier choices like multigrain rice, milk, soy milk, and vegetable soups. These foods not only provide rich nutrition but also help stabilize blood sugar and reduce the burden on the islets.

Protecting Islet Function: Four Most Effective Methods
Faced with the ongoing damage to islet function, people with diabetes are not helpless. The following four suggestions may provide guidance on your path to health:
1. Lower Blood Sugar Quickly to Awaken Pancreatic Beta Cells: The period immediately after a diabetes diagnosis is the golden window for treatment. If blood sugar can be quickly lowered to normal levels during this time through intensive insulin or medication therapy, it can effectively awaken dormant or weakened pancreatic beta cells, revitalizing them to continue secreting insulin.
2. Maintain Long-Term Blood Sugar Stability: Prolonged hyperglycemia is a "chronic poison" for pancreatic beta cells. Therefore, people with diabetes need to monitor their blood sugar regularly, ensuring it fluctuates within the normal range. If blood sugar control remains suboptimal for over a week, medical attention should be sought promptly to adjust the treatment plan.

3. Reduce Weight to Lessen the Burden on Islets: Obesity is an "accelerator" for diabetes. Losing weight, especially reducing abdominal fat, can significantly decrease insulin resistance and lessen the burden on pancreatic beta cells. Achieving healthy weight loss through a balanced diet and moderate exercise is an important means of protecting islet function.
4. Exercise One Hour After Meals: Exercise is a "good medicine" for diabetes management. Engaging in moderate exercise, such as brisk walking, jogging, or swimming, one hour after meals can effectively consume excess sugar in the body, lower blood sugar levels, and "lighten the load" on islet cells. Simultaneously, exercise can improve the body's insulin sensitivity, making pancreatic beta cells work more efficiently.
Knowledge Extension: How Is Islet Function Measured?
The measurement of islet function plays a pivotal role in the diagnosis, treatment, and monitoring of diabetes. Islet function primarily refers to the ability of pancreatic endocrine cells (mainly pancreatic beta cells) to secrete insulin and glucagon, hormones crucial for maintaining the body's blood sugar balance. The following are several main methods for measuring islet function and their detailed explanations.
1. Fasting Blood Glucose Measurement
Fasting blood glucose measurement is one of the most fundamental methods for assessing islet function. Before this test, the subject must fast for at least 8 hours to ensure the measured blood glucose value accurately reflects the islets' ability to regulate blood sugar. Normally, an adult's fasting blood glucose level should be between 3.9-6.1 mmol/L. If fasting blood glucose consistently exceeds this range, it may indicate abnormal islet function, meaning insufficient insulin secretion by pancreatic beta cells or impaired insulin action, leading to blood sugar regulation imbalance.
2. Oral Glucose Tolerance Test (OGTT)
The oral glucose tolerance test is an important means of assessing the islets' response to a glucose load. The subject must drink a solution containing 75g of glucose in a fasting state, and venous blood is drawn at 30 minutes, 1 hour, 2 hours, and 3 hours after ingestion to measure blood glucose concentration. Normally, blood sugar returns to normal levels rapidly within 2-3 hours after ingestion, while insulin levels peak within 30-60 minutes and then gradually decline. If the blood glucose concentration remains above 7.8 mmol/L after 2 hours, it may indicate impaired islet function, suggesting insulin resistance or insufficient insulin secretion.
3. Insulin Release Test
The insulin release test involves giving the subject a certain glucose load (such as oral glucose or a steamed bun meal) to stimulate pancreatic beta cells to secrete insulin, then measuring serum insulin concentration at different time points. This method can directly reflect the reserve and secretory functions of pancreatic beta cells. Normally, insulin levels rise rapidly after glucose ingestion, reach a peak within a certain period, and then gradually decline. Delayed insulin secretion or a reduced peak may indicate decreased islet function.

4. C-Peptide Measurement
C-peptide is a polypeptide substance produced by the cleavage of proinsulin and is secreted simultaneously with insulin in equimolar amounts. Since C-peptide is not affected by the liver's first-pass effect or exogenous insulin, C-peptide measurement is a sensitive indicator for evaluating islet function. By measuring the concentration of C-peptide in the blood, the functional status of pancreatic beta cells can be assessed more accurately. Normally, fasting C-peptide levels are low, rising rapidly after glucose ingestion and reaching a peak within a certain period. Abnormal C-peptide levels may indicate impaired islet function.
5. Glycated Hemoglobin Measurement
Glycated hemoglobin is a product formed by the combination of hemoglobin in red blood cells and sugars in the serum. Its concentration reflects the average blood glucose level over the past 2-3 months. This indicator is significant for understanding a patient's long-term blood glucose control and indirectly assessing islet function. By regularly testing glycated hemoglobin, doctors can determine whether the patient's treatment plan is effective and if adjustments to the treatment strategy are needed.
6. Insulin Antibody Detection
Insulin antibody detection is primarily used to determine the presence of diseases such as autoimmune insulitis. Autoimmune insulitis is a disease involving islet function damage caused by an autoimmune reaction, where the body produces antibodies against insulin, affecting its efficacy. By detecting the level of insulin antibodies in the blood, doctors can determine if the patient has such a condition and formulate an appropriate treatment plan accordingly.