If a diabetic patient loses sensation in any of these four areas on the sole of the foot, it indicates a high risk of diabetic foot.
"Doctor, how did I get such a big wound on my foot without even feeling it?" At the outpatient clinic of Lanzhou Ruijing Diabetes Hospital, Chief Physician Song Shuhua, Deputy Director and outpatient specialist, often hears such shocked questions from patients. Winter is the high-incidence season for diabetic foot. Many patients seek medical attention for a small foot ulcer, only to find it has progressed to a severe infection or even risks amputation.
Facing this one of the most dreaded complications of diabetes, Chief Physician Song Shuhua always emphasizes with concern: "Diabetic foot does not strike suddenly; it has a clear 'prelude'—the high-risk diabetic foot. If we can identify and intervene decisively at this stage, the vast majority of tragedies can be avoided."
01
The Silent Warning: Understanding the High-Risk Diabetic Foot
Many diabetic patients focus only on blood sugar numbers, overlooking the early warning signs from their feet. Diabetic foot results from the combined effects of long-term hyperglycemia leading to neuropathy and lower limb vascular disease. It does not occur overnight but is a gradual process.
Before foot ulcers and gangrene develop, there is a critical window period—the "high-risk diabetic foot." At this stage, patients may only experience numbness, coldness, a crawling sensation like ants, or diminished sensitivity to temperature and pain in their feet.
The greatest danger lies precisely in this 'numbness'. Chief Physician Song Shuhua explains that due to sensory nerve damage, patients often remain unaware when their feet are injured (e.g., rubbed raw by shoes, scalded by hot water, or punctured by a foreign object). Minor wounds are highly susceptible to infection and ulceration in an ischemic and high-glucose environment, eventually spiraling out of control.
Therefore, recognizing whether one is already in a "high-risk foot" state is the most crucial first step in preventing diabetic foot. Fortunately, there is a simple and effective method that can be done at home.
02
Simple Self-Test: The 4-Point Method for Screening High-Risk Foot
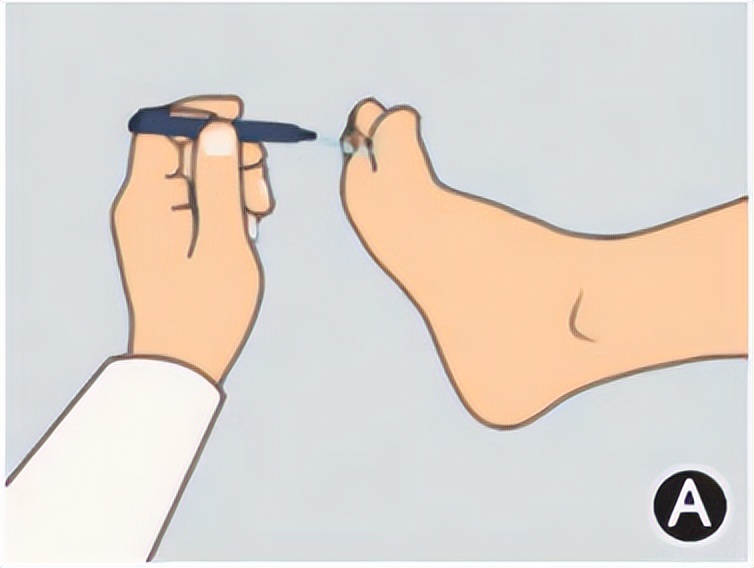
Chief Physician Song Shuhua explains that the internationally recognized "10-gram monofilament test" is the gold standard for screening diabetic peripheral neuropathy and identifying high-risk foot. Its accuracy and predictive value have been confirmed by extensive research. Patients can easily perform this test at home.
The tool you need is very simple: a standard 10-gram monofilament (which can be obtained by consulting the hospital's endocrinology department or a podiatrist). If unavailable, there are some alternatives, such as: a single plastic bristle from a small bed whisk or a fine filament from a razor cleaning brush, as their stiffness approximates 10 grams of force.
The test sites are key: Please locate the following four specific areas on the sole of the foot. These are the most weight-bearing and ulcer-prone regions:
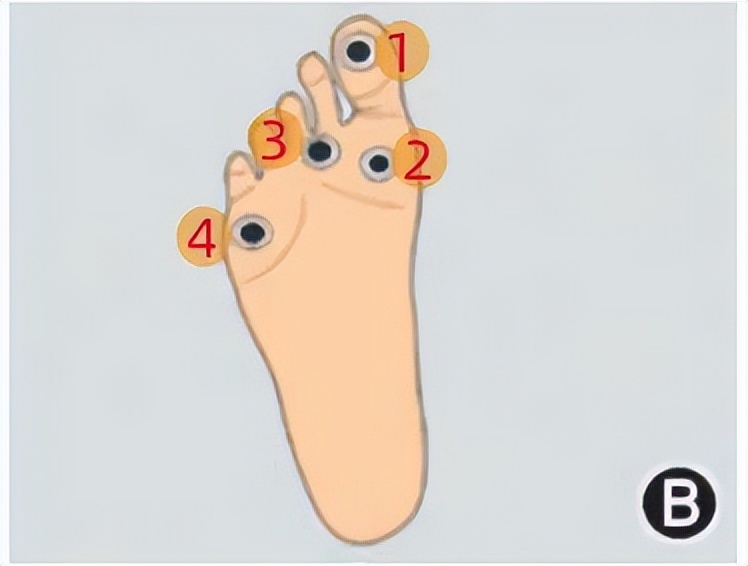
- The plantar surface of the big toe
- The first metatarsal head (the ball-shaped prominence at the base of the big toe)
- The third metatarsal head (the middle of the sole)
- The fifth metatarsal head (the ball-shaped prominence at the base of the little toe)
Correct testing method: Ask a family member for assistance and close your eyes. Place the monofilament perpendicular to the test site and press firmly until it bends into a "C" shape, holding for 1-2 seconds. You need to purely perceive "the pressure of being touched," not guess.
How to interpret the results: Test each site three times. If at any one location, you fail to feel the pressure more than twice, it strongly suggests your foot has entered a "high-risk" state, indicating diminished or lost protective sensation.
"Never underestimate this simple test," Chief Physician Song Shuhua points out seriously. "It can effectively predict the risk of future foot ulcer development. Once an abnormality is detected, it is an alarm bell from your body, and immediate action is necessary."
03
Professional Intervention: What to Do After Identifying High-Risk Foot
If your self-test results are abnormal, do not panic, but do not take it lightly either. Chief Physician Song Shuhua provides a clear action plan:
Step 1: Seek Professional Assessment Immediately. Visit the endocrinology department or a diabetic foot specialty clinic at a hospital as soon as possible. The doctor will conduct a more comprehensive examination, including assessments of vibration sense, temperature sense, ankle reflexes, and evaluate lower limb vascular status (e.g., ankle-brachial index) to determine the extent of the condition.
Step 2: Receive Professional Foot Care Education and Guidance. Learn the correct methods for washing, drying, and trimming toenails. Understand how to choose appropriate footwear and socks (loose, breathable, seamless, with a smooth interior).
Step 3: Establish and Implement a Daily Foot Inspection Routine. This must become a daily habit, like checking blood sugar. Every day in good light, inspect both feet and between toes for redness, swelling, blisters, ulcers, calluses, or color changes. If you cannot see clearly, use a mirror or ask a family member for help.
04
Winter Special Care: Putting 'Protective Clothing' on Diabetic Feet
Winter, with its dry, cold climate and vasoconstriction, is a critical period for diabetic foot protection. Chief Physician Song Shuhua specifically outlines key winter foot care points for people with diabetes:
1. Wash Feet with Warm Water, Avoid Soaking or Scalding. Wash feet daily with warm water below 37°C for no more than 10 minutes. Test the water temperature with your elbow or a thermometer; never use your feet. After washing, gently dry with a soft, absorbent, light-colored towel, especially between toes.
2. Maintain Moisture, Prevent Cracking. Dry foot skin is prone to cracking. After washing, apply urea cream or moisturizer to keep skin hydrated, but avoid applying between toes.
3. Keep Warm Strictly, Stay Away from Direct Heat Sources. Wear warm cotton socks and loose shoes. Absolutely avoid using hot water bottles, electric blankets, or heaters directly on feet, as diminished sensation makes low-temperature burns highly likely.
4. Choosing Footwear and Socks is Crucial. Choose shoes with soft uppers, ample interior space, and good breathability. Always check inside shoes for foreign objects before wearing. Socks should be light-colored, seamless, and made of absorbent cotton to easily detect any foot discharge or bloodstains.
5. Improve Circulation, Promote Blood Supply. Under a doctor's guidance, perform non-weight-bearing exercises such as ankle pump exercises (pointing and flexing feet) to promote lower limb blood circulation. Avoid crossing legs when sitting to prevent vascular compression.
Chief Physician Song Shuhua concludes: "Managing diabetes cannot focus solely on the glucose meter. Your feet are a mirror reflecting the health of your entire vascular and nervous system. A simple self-test and daily persistence can build a solid defense line against diabetic foot."