Winter influenza season: how should people with diabetes prevent it? Expert Ren Shuhong offers tips!
The north wind howls ❄️, temperatures plummet, and with winter comes flu season. People with diabetes need to take extra care of their health. Today, doctor to explain how people with diabetes can prevent the flu in winter and how to manage blood glucose if they do get the flu.

Why should people with diabetes be especially vigilant about influenza?
Director Ren Shuhong pointed out: “Because people with diabetes have long-standing hyperglycemia, their immune system function is relatively weaker and resistance is reduced, making them more susceptible to influenza virus infection. Once infected, the illness is often more severe than in the general population, recovery takes longer, and they are more prone to complications such as pneumonia.”
More importantly, infection causes increased secretion of stress hormones, which counteract the action of insulin, leading to a sharp rise in blood glucose levels and increasing the risk of acute diabetic complications.
To prevent influenza, Director Ren gives five major recommendations ✨
1️⃣ Get the influenza vaccine promptly
“Annual influenza vaccination is the most effective measure to prevent influenza,” Director Ren emphasized. “Patients with diabetes belong to a high-risk group and should be given priority for vaccination. It is recommended to complete vaccination before the start of the flu season (usually October).”

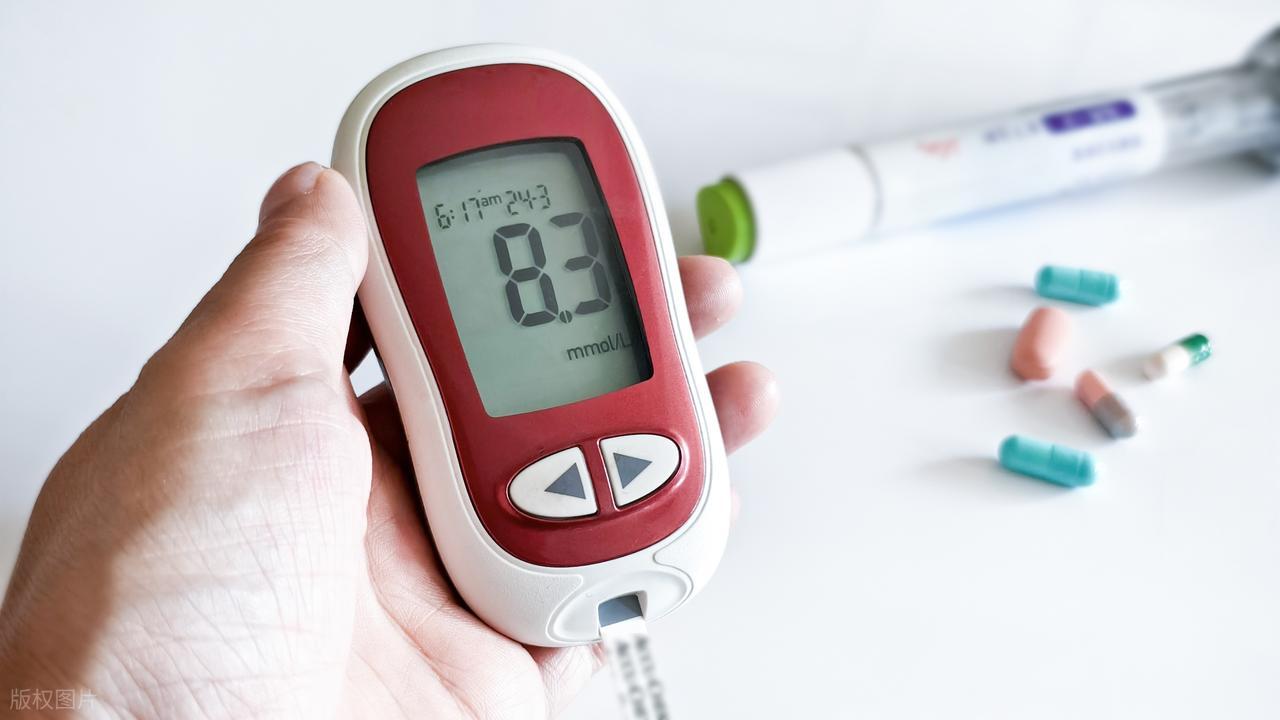
2️⃣ Strengthen blood glucose monitoring
Winter brings large temperature fluctuations, and the body’s metabolism will adjust accordingly. Director Ren suggested, “Increase the frequency of blood glucose monitoring, especially fasting and postprandial glucose, to ensure blood glucose control remains within a stable range. Good glycemic control itself is the basis for strengthening immunity.”
3️⃣ Pay attention to personal protection
Wash hands frequently using soap or handwash, scrubbing for at least 20 seconds
Avoid visiting crowded public places
Wear a mask when necessary
Keep indoor air ventilated; open windows 2–3 times a day
4️⃣ Maintain a balanced diet and nutrition
“Do not take supplements blindly in winter,” Director Ren reminds, “maintain a balanced diet, moderately increase intake of high-quality protein such as fish, poultry, eggs, and dairy, while ensuring consumption of fresh vegetables and fruits to supplement antioxidants like vitamin C.”
5️⃣ Moderate exercise and keep warm ♂️
Choose indoor exercises such as tai chi, yoga, or indoor walking. When going outside, keep warm, especially the head, neck, and feet. Director Ren specially reminds: "Keeping the feet warm is particularly important for people with diabetes, and they should check their feet daily to prevent diabetic foot."
What if you get the flu—how should you manage blood glucose?
Even with precautions, it is still possible to contract influenza. Director Ren points out that blood glucose management becomes even more critical at this time:
1. Strengthen monitoring and adjust protocols
"During infection, increase the frequency of blood glucose monitoring to at least 4–6 times per day," Director Ren said. "If blood glucose remains persistently above 13.9 mmol/L, or if nausea, vomiting, abdominal pain, or rapid deep breathing occur, seek medical attention immediately."
2. Do not arbitrarily stop medication
"Some patients think that if they can't eat they should reduce or stop hypoglycemic medications on their own; this is extremely dangerous!" Director Ren warned sternly. "During infection, even with reduced food intake, stress responses can cause blood glucose to rise; be sure to adjust medications according to medical advice."
3. Ensure adequate fluid intake
Fever and sweating can cause fluid loss, leading to hemoconcentration and subsequent blood glucose elevation. Director Ren suggests: "Ensure a daily intake of 1500–2000 mL of fluids, unless fluid restriction is required due to cardiac or renal complications."
4. Adjust diet and ensure adequate nutrition
"Even with poor appetite, you should try to eat." Director Ren recommends, "You can eat small, frequent meals and choose easily digestible foods such as porridge, noodles, and steamed eggs. If you are completely unable to eat, seek medical attention promptly to consider intravenous fluids and nutritional support."
5. Pay attention to drug interactions
Director Ren specially reminds: "Many cold medicines contain components that affect blood glucose, such as certain cough syrups with high sugar content, and some antipyretic/analgesic drugs may affect liver and kidney function. Before using any medication, consult a physician or pharmacist."
When should you seek immediate medical attention?
Director Ren Shuhong listed warning signs for people with diabetes who should seek immediate medical attention after contracting influenza:
Blood glucose persistently above 13.9 mmol/L and uncontrolled despite medication adjustments
Nausea, vomiting, abdominal pain
Deep, rapid breathing with a rotten apple odor (possible ketoacidosis)
Confusion, drowsiness
High fever persisting for more than 3 days
Chest tightness, difficulty breathing
Winter blood-glucose control tips
Director Ren added some practical recommendations for blood sugar control in winter:
Sunlight exposure decreases in winter; it may be appropriate to supplement with vitamin D
Maintain a regular routine and avoid staying up late
Learn to manage emotions and avoid depression caused by seasonal changes that can affect blood glucose
Regular follow-up examinations, including multiple indicators such as blood glucose, blood pressure, and blood lipids
"Diabetes management is a long-term battle, and winter is a critical campaign within it," summarized Director Ren Shuhong. "With scientific prevention and appropriate response, people with diabetes can smoothly get through the flu season and enjoy a healthy, warm winter."