Cervical Cancer Screening How to Choose Between TCT and HPV Learn in 1 Minute and Avoid 90 of the Pitfalls
First, Understand: The Two Tests Are Like "Investigation Partners" with Different Roles
Patients ask every day in the outpatient clinic: "Doctor, what exactly do TCT and HPV check?" In fact, the two are the golden combination for cervical cancer screening, but their roles are completely different:
HPV testIdentify the "cancer-causing suspects." Check whether the cervix is infected with high-risk HPV viruses (especially types 16/18, which account for 70% of cervical cancer causes) to see if there is a "motive for the crime." However, a positive result does not equal cancer—80% of women will be infected, and most can be cleared by the immune system. Only persistent infection for more than 2 years poses a risk.
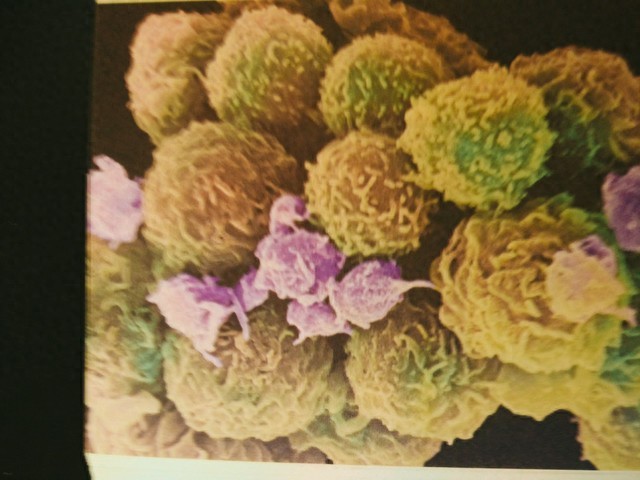
TCT examinationLook at "cell victims". Use a specially designed brush to collect cervical cells and observe under a microscope for any abnormal lesions, like taking a "close-up" of the cells to determine if "traces of damage" have already appeared. However, it has limitations; when HPV infection is recent, the cells may not have mutated yet, potentially leading to missed diagnoses.
II. Key Issue: Age-Specific Considerations Lead to Significantly Different Choices!
According to the latest clinical guidelines, the screening program is categorized into three population groups:
1. 21-29 years oldFor TCT alone, once every 3 years. HPV infections in this age group are mostly transient, and TCT can directly reflect cell status, offering the best cost-effectiveness.
2. 30-65 years oldThe preferred option is combined TCT+HPV screening (once every 5 years), or TCT alone (once every 3 years). The combined screening achieves an accuracy rate of over 95%, enabling simultaneous detection of the "culprit" and assessment of the "damage."
3. Over 65 years oldScreening can be discontinued if there have been normal screenings for the past 10 years and no history of precancerous lesions.
⚠️ High-risk groups (multiple partners, smoking, low immunity) need to shorten intervals and undergo additional HPV testing as advised by a doctor.
III. Pitfall Avoidance Guide: Steer Clear of These 4 Common Misconceptions!
1. "No need for screening after receiving the HPV vaccine?"Wrong! Vaccines only protect against specific subtypes and cannot provide full coverage, so screening must be consistently maintained.
2. "Is Everything Fine with a Normal TCT Result?"High risk of missed diagnosis! If HPV infection is recent and cells have not yet mutated, TCT may show normal results.
3. "Does a Positive HPV Test Mean Cervical Cancer?"Completely wrong! Only indicating risk requires further assessment with TCT, and most people can clear the infection on their own.
4. "Is it always safe if both are normal?"Screening tests have an expiration date, as viral infections may occur before the next examination, making regular testing essential.
IV. Pre-examination Precautions: 3 Factors That May Affect Results!
Time: 3-7 days after menstruation ends is optimal; avoid during menstruation.
Preparation: Avoid sexual intercourse and vaginal medication/douching for 24 hours prior.
Reminder Both tests can be sampled simultaneously the entire process is painless and takes 2 minutes