Normal TCT but Diagnosed with Cervical Cancer? Qilu Doctors Reveal 3 Truths, Avoid These Screening Pitfalls
Doctor, my TCT was normal last year, how could I be diagnosed with cervical cancer this year? This is the most heartbreaking question at the HPV clinic of Qilu Hospital. Last week, 46-year-old Ms. Li, who came for a consultation, is a typical case: in 2023, her TCT indicated no abnormalities, but this year, after experiencing bleeding following intercourse and undergoing a re-examination, she was diagnosed with stage IB cervical cancer. In fact, although such cases are rare, they reveal critical gaps in screening. Today, we will explain everything clearly to help you avoid fatal misconceptions.
I. First Understand: Why Can TCT Normal Results Miss Diagnoses? 3 Core Reasons
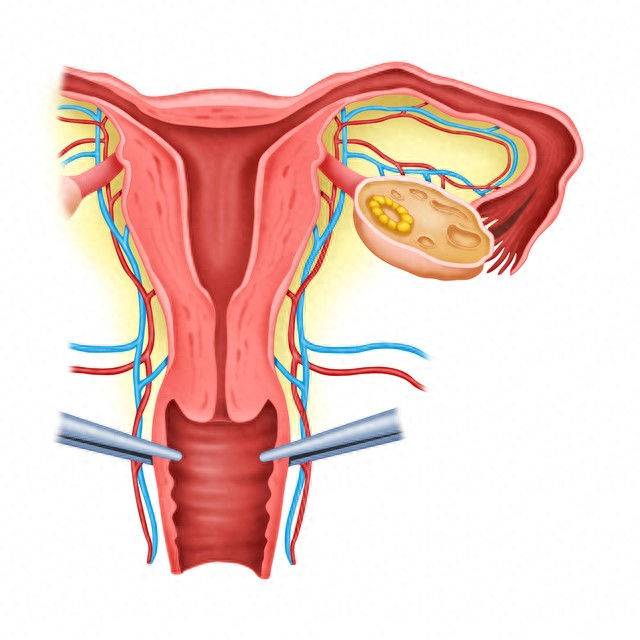
1. Sampling "Almost Missed": The "Blind Spot" of the Cervix Was Not Sampled
TCT uses a small brush to collect cells from the surface of the cervix, similar to a "sampling test." If cancer cells are hidden deep within the cervical canal or the lesion is very small, the brush may miss them. In Ms. Li's case, the lesion was located inside the cervical canal, and last year's sampling did not reach it, resulting in a false negative TCT result. This situation is more common in postmenopausal women—declining estrogen levels cause cervical atrophy, deepening the cervical canal and increasing the difficulty of sampling.
2. Detection "Earlier": Cancer Cells Not Yet "Visible"
The development of cervical cancer goes through the process of "HPV infection → precancerous lesions → cancer," which may take up to 10 years. If during a TCT examination, the cancer cells are still in the "budding stage" (such as early invasive cancer), the cell morphology differs little from normal cells, making them difficult to identify under a microscope. Just as it is hard to distinguish between crops and weeds with the naked eye when seeds have just sprouted, TCT may also lead to misjudgment.
3. Cancer "Special Considerations": Rare Types Prone to Misdiagnosis
90% of cervical cancers are squamous cell carcinomas, and TCT has a high detection rate for squamous cell carcinoma. However, its sensitivity decreases for rare types such as adenocarcinoma and small cell carcinoma. These cancers often originate in the endocervical canal, with early symptoms being inconspicuous, making TCT prone to "overlooking" them. By the time symptoms appear, the cancer may have progressed to an intermediate or advanced stage.
II. Key Reminder: Do Not Treat TCT as the "Sole Shield Against Cancer"
Many people believe that "a normal TCT result means safety," which is a fatal misconception! Clinical data show that the missed diagnosis rate of TCT screening alone is about 10%-15%, while the accuracy of combined HPV and TCT screening can reach over 95%.
HPV is the "culprit" of cervical cancer, while TCT examines "whether the cells have been harmed." If only TCT is performed, even if the cells appear normal, persistent infection with high-risk HPV types may lead to the development of lesions within the next 1-2 years. Ms. Li experienced a missed diagnosis precisely because she did not undergo HPV testing, overlooking the risk of her long-term infection with HPV type 18.
III. Three "Hard Cancer Prevention Recommendations" from Qilu Doctors
1. "Combined Screening" is a Must for Those Over 30HPV and TCT should be performed together every 5 years; for high-risk groups (multiple partners, smoking, low immunity), the interval should be shortened to every 3 years. This is currently the most reliable screening protocol.
2. Normal TCT but with symptoms, do not tough it outIf there is bleeding after intercourse, postmenopausal bleeding, or blood in vaginal discharge, even if a TCT has just been performed, a colposcopy + biopsy should be promptly conducted to avoid missing hidden lesions.
3. Postmenopausal Women Should Not Neglect ScreeningPostmenopausal cervical atrophy increases the risk of sampling errors. It is recommended to undergo combined screening every 3 years, with endocervical curettage added if necessary to ensure comprehensive lesion coverage.
Finally, I want to say: TCT is an excellent "initial screening tool," but it is not a "universal shield." Only through scientific combined screening and paying attention to abnormal symptoms can cervical cancer truly be prevented. Ms. Li has recovered well after surgical treatment, but if she had undergone combined screening earlier, intervention could have been made at the precancerous stage.
How long has it been since your last cervical cancer screening? Was it a standalone TCT or a combined screening? Leave a comment below, and I'll help you analyze your risk.