What does high-risk HPV for cervical cancer mean? Not all high-risk types are the same; these 3 points are most critical
"Doctor, my test shows HPV high-risk positive! Does that mean cervical cancer is imminent?" Every day in clinic I meet patients terrified by the words "high-risk" — many think "high-risk type = precancerous," not realizing there are more than 20 high-risk HPV types with wildly different danger levels, and the vast majority of infections clear spontaneously. Today, as a gynecologist, I'll explain the truth about high-risk HPV in one go: it is the "prime suspect" that causes cervical cancer, but not the "convicting evidence." Only a "specific high-risk type + persistent infection + cellular abnormality" will lead to cervical cancer. Read this and you'll fully understand without panic.

First, a reassurance: 32-year-old Ms. Wang tested positive for HPV33 (high-risk) and was so frightened she lost sleep for a week; her TCT was normal, and after following my immune-modulating plan she tested negative after 6 months; 45-year-old Aunt Li was HPV16 (high-risk) positive for 2 years, TCT showed cellular abnormalities, and timely colposcopy + biopsy found low-grade lesions—after intervention she also recovered within a year. This shows that high-risk HPV is only a "risk signal," not a "cancer verdict."
1. First understand: what exactly is "high" about high-risk HPV?
HPV (human papillomavirus) is classified into "high-risk" and "low-risk"; the core difference is "whether it is carcinogenic":
High-risk HPV: like a "latent carcinogenic assassin," it can reside in the cervix long-term, potentially inducing cellular malignant transformation and ultimately causing cervical cancer, vaginal cancer, etc.
Low-risk HPV (types 6, 11, etc.): like "harmless hooligans," they only cause condyloma acuminata and are not carcinogenic.
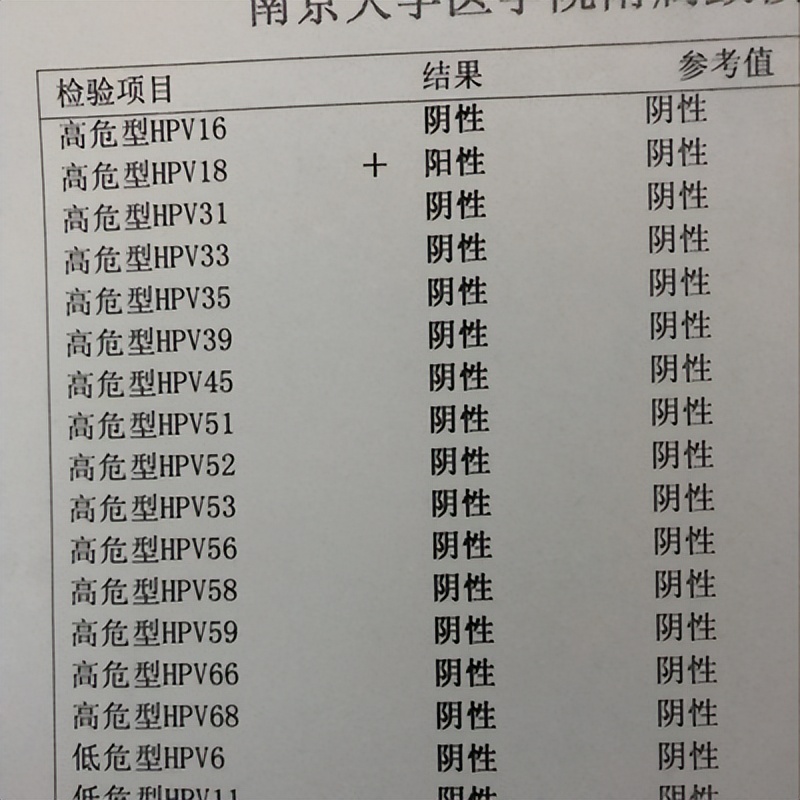
Key point: Among high-risk HPV types, there are "top-tier dangerous agents" and "ordinary dangerous agents":
Top high-risk types (16, 18): responsible for 70% of cervical cancers, with the strongest carcinogenic potential; even if TCT is normal, colposcopic evaluation is still recommended.
Other high-risk types (31, 33, 45, 52, 58, etc.): carcinogenic risk is secondary, accounting for 20%–30% of cervical cancer etiology; intervention decisions should be made in conjunction with TCT results.
Clinical data show: 80% of women will be infected with HPV at some point in their lives, of which high-risk infections account for about 30%; however, over 90% can be cleared by their own immune system within 1–2 years. Only "persistent infection lasting more than 2 years" will gradually progress to lesions.
2. How do high-risk HPV types cause cervical cancer? Just 3 steps, each step can be intervened upon
The occurrence of cervical cancer is not a "sudden event," but the result of high-risk HPV "advancing step by step." The whole process takes 5–10 years, and each step can be interrupted:
Step 1: Infection with high-risk HPV: transmitted through sexual activity (rarely via indirect transmission), the virus enters cervical cells and "latently" persists; at this stage there are no symptoms and TCT is normal;
Step 2: Persistent infection for more than 2 years: poor immunity and repeated cross-infections prevent the virus from being cleared, beginning to continuously stimulate cervical cells;
Step 3: Cervical cell abnormalities → lesions → cancer: the virus continuously damages cellular DNA, initially causing "low-grade lesions," then progressing to "high-grade lesions" (precancerous lesions), and only eventually possibly developing into cervical cancer.
Key reminder: There is a long "reversible period" between "persistent infection" and "cancer"—most low-grade lesions can heal spontaneously, and high-grade lesions have a cure rate over 95% with conization; if detected in time, progression to cancer can be completely prevented.
3. If a high-risk HPV test is positive, respond according to these 3 situations to stay steady and calm
Situation 1: Top high-risk types (16, 18) + any TCT result
Management: Proceed directly to colposcopy + biopsy (gold standard); even if TCT is normal, occult lesions may exist;
Case: 28-year-old Ms. Zhang was HPV16 positive, TCT normal; colposcopic biopsy found low-grade lesions within the endocervical canal, which reverted to negative after 6 months of immune regulation.
Situation 2: Other high-risk types (33, 52, etc.) + TCT normal
Management: No treatment required. Recheck HPV + TCT every 6 months; if both tests are negative for 2 consecutive years, switch to annual testing.
Key points: Enhance immunity (sleep at least 7 hours, eat more protein, engage in moderate exercise). Use condoms during intercourse to avoid cross-infection.
Scenario 3: Any high-risk type + abnormal TCT (e.g., ASC-H, LSIL)
Management: Perform colposcopy with biopsy immediately and manage according to the results:
Low-grade lesions: observation + immune regulation, recheck every 6 months;
High-grade lesions: perform cervical conization; after surgery, still need a recheck every 6 months for 2 years with no abnormalities before returning to routine screening.
4. Three common misconceptions — avoid them!
“High-risk type positive = cancer” → Wrong! It is only an infection; cancer requires two more steps — “persistent infection + cellular abnormalities” — and the probability is less than 0.1%;
"Positive test alone does not mean surgery" → False! A simple positive result does not require surgery; surgery will damage the cervical mucosa and actually reduce resistance. Only biopsy-proven lesions require surgery;
"Once negative, no more screening is needed" → False! HPV does not confer lifelong immunity and reinfection with other high-risk types is possible. Women aged 21 and over who are sexually active need lifelong regular screening.
5. To prevent high-risk HPV infection, do these 2 things for the best cost-effectiveness
HPV vaccination: can be administered from 9–45 years of age. The bivalent and quadrivalent vaccines cover types 16 and 18 (the core oncogenic types); the nine-valent vaccine covers more high-risk types. Earlier vaccination provides earlier protection;
Standardized screening: ages 21–29 should have a TCT every 2 years; after age 30, an HPV+TCT every 1–3 years. This is key to detecting early infections and lesions.
Finally, I want to tell you: high-risk HPV is not a “monstrous flood,” but a “health warning” sent by your body. Its carcinogenic process is long and can be intervened upon. What is truly dangerous is not the infection itself, but blind panic and neglecting screening.
If you are currently anxious because you have a positive high-risk HPV report, don’t panic. First, check the genotype and the TCT result carefully, and tomorrow take the report to the gynecology department of a reputable hospital for consultation — the doctor will help you develop a personalized plan. Your body is capable of overcoming the virus; what you need to do is trust it and support it, not be frightened by the words “high-risk.”
Remember: respond scientifically — high-risk HPV is completely controllable, and cervical cancer can be effectively prevented. Share this with the women around you; don’t let unnecessary anxiety wear you down!