Recurrent Candidal Vaginitis? Doctor: Don’t Rely on Medication Alone! Do These 4 Things to Eradicate It and Prevent Recurrence
What to do if vulvovaginal candidiasis keeps recurring?
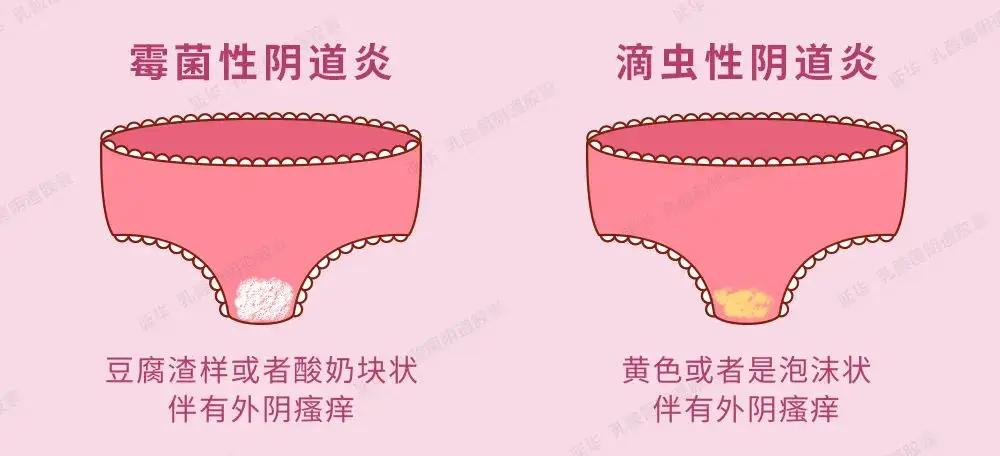
"Doctor, my vulvovaginal candidiasis has flared up again! My vulva itches so badly I can’t sleep, the discharge is like cottage cheese, it gets better with medication and then comes back as soon as I stop—how can it be cured for good?" Every day in clinic I see women tormented by recurrences — clinical data show about 5% of women experience "recurrent vulvovaginal candidiasis" (≥4 recurrences in 1 year). Many fall into a vicious cycle of "medicate — improve — relapse" and even lose confidence in treatment. Today, as a gynecologist, I will analyze the core reasons for recurrence and share four "root-cutting strategies" to avoid repeated "medication lists" and address the problem at its source.
Key conclusion first: recurrence of vulvovaginal candidiasis is not "the drugs don’t work," but "treatment is not standardized + triggers are not eliminated." Ms. Chen, 32, had recurrences for 3 years and tried multiple suppositories without success. Following my plan of "standardized medication + lifestyle adjustments," she has had no recurrence for 1 year. She said, "Turns out before we only treated the symptoms, not the root cause."

1. First, understand: Why does it recur? 3 core reasons
Incomplete treatment allows Candida to "hide"
This is the most common reason! Many people stop medication as soon as symptoms disappear without completing the "consolidation course" — the fungus is not completely eradicated and can hide in the folds of the vaginal mucosa, ready to return when the body's resistance drops. For example, uncomplicated vaginitis requires 7–14 days of treatment, while recurrent cases need consolidation for 3–6 months; stopping medication on your own is equivalent to "leaving the fungus a way to live."
Imbalance of the vaginal microbiota — too few "good bacteria"
There are "good bacteria" (Lactobacilli) and "bad bacteria" in the vagina; fungi are a type of "bad bacteria." Long-term antibiotic use and frequent vaginal douching will kill Lactobacilli, leading to reduced vaginal defenses and allowing fungi to proliferate easily. Ms. Chen's recurrences worsened the more she used potent suppositories each time, precisely because the microbial balance was destroyed.
Triggers not eliminated, repeatedly "provoking" the fungus
Many habits in daily life can cause yeast infections to recur:
Eating too many sweets: high blood sugar increases vaginal glycogen; yeast “feeds on sugar” and can proliferate rapidly;
Wearing tight pants / synthetic-fiber underwear: poor breathability and increased sweating create a “breeding ground” for yeast;
Partner not treated simultaneously: yeast can be transmitted through sexual activity; after you are treated, yeast on your partner can reinfect you;
Staying up late, high stress: immunity declines, giving Candida an opportunity.
2. Eradication plan: Do these 4 things — 10 times more effective than medication alone
Standardized treatment: use medication according to the “type,” do not stop medication on your own
Simple relapse (2–3 times per year): after symptoms disappear, continue medication for 7 days to consolidate, then use medication for 3 days before and after the next menstruation, for 3 consecutive cycles;
Recurrent (≥4 times per year): first wash the vulva with water (do not douche), insert clotrimazole suppositories / miconazole suppositories into the vagina once daily for 14 consecutive days; thereafter use medication once weekly for consolidation for 3–6 months; severe cases require oral fluconazole (follow medical advice; contraindicated in pregnancy).
Key point: Do not stop medication during treatment; even if menstruation occurs you can pause, then continue and complete the full course after menstruation ends.

Replenish "good bacteria" to rebuild the vaginal defense barrier
In the later stage of treatment, under a doctor's guidance use "Lactobacillus vaginal capsules", 1 capsule daily for 10 consecutive days — Lactobacillus can regulate vaginal pH, inhibit fungal growth, and is equivalent to "reinforcing troops" in the vagina, enhancing resistance from the root. Ms. Chen supplemented with Lactobacillus during the late stage of medication; after the flora balanced, the fungus never recurred.
Eliminate triggers: these habits must change, otherwise treatment is in vain
Diet: avoid high sugar! Stop milk tea, cakes, and sugary drinks; daily sugar intake ≤ 20 g (about 1 sugar cube); eat more vegetables and high-quality protein to boost immunity;
Clothing: wear pure cotton underwear, change daily, scald and sun-dry after washing (do not use a dryer; fungi hate high temperatures); avoid tight jeans and synthetic leggings, keep the vulva well ventilated;
Hygiene: Do not douch the vagina with cleansing solutions; wash the vulva daily with warm water only; after defecation wipe from front to back to avoid contaminating the vagina with anal Candida.
Treat the partner as well: Men should apply clotrimazole cream to the glans and the inner surface of the foreskin once daily for 7 consecutive days; use condoms during the treatment period to avoid cross-infection.
Boost immunity: Let the body “fight” Candida on its own
Fungi Prefer to “Attack” People with Poor Immunity:
Avoid late nights: ensure 7–8 hours of sleep daily, go to bed before 23:00;
Moderate exercise: brisk walk 30 minutes daily, or dance in the square twice a week to activate immune cells;
Use antibiotics sparingly: unless a doctor clearly indicates they are needed, do not take antibiotics on your own to avoid killing Lactobacilli.
3. Three common misconceptions — don’t let recurrence get worse with treatment
"Stop medication when symptoms disappear to save medicine"
Wrong! Disappearance of symptoms does not mean the fungus has been eradicated. Stopping medication on your own is the number-one culprit for recurrence; you must complete the full course, including consolidation therapy.
"Using vaginal douches can wash the fungus away"
Wrong! Douching disrupts the vaginal microbiome balance and weakens defenses, which actually allows the fungus to multiply faster. Rinsing the external vulva with warm water is sufficient.
"Relapse, so switch to a more expensive drug"
Wrong! Medications are not "the more expensive the better"; the key is proper use. Frequently switching to more potent drugs can lead to fungal resistance, making subsequent treatment more difficult.
4. Special circumstances: seek medical attention promptly if any of the following occur
Relapse more than 4 times per year, or no improvement after 14 days of medication;
Accompanied by severe abdominal pain, fever, or blood-streaked discharge;
Pregnant women, patients with diabetes, and immunocompromised individuals (e.g., long-term steroid users): after recurrence do not self-medicate; you need a physician to devise a personalized plan.
Finally, I want to tell you: recurrent vulvovaginal candidiasis is not an "incurable disease"—it means you haven't found the right approach. As long as you follow "standardized medication + restore beneficial bacteria + remove precipitating factors + boost immunity," the vast majority of people can achieve a complete cure. Don’t be tormented by recurrences, and don’t switch medications blindly; follow the plan above and persist for 3–6 months, and you can rid yourself of the Candida problem.
If you are currently troubled by recurrences, don’t be anxious—go to the hospital tomorrow for a routine vaginal discharge test so the doctor can determine the type, then treat according to the standard protocol—your persistence will eventually be rewarded with health!