How to Treat Vaginitis Effectively? Don’t Use Medications Blindly! First Classify into 4 Types, Treat According to Symptoms to Prevent Recurrence
How to Effectively Treat Vaginitis
"Doctor, my vaginitis is acting up again! My vaginal discharge is yellow and itchy. I bought washes and suppositories myself, but the more I use them the worse it gets. How should it be treated properly?" In the clinic every day I see patients who misuse medications — vaginitis is not a "single disease," but four different types of "combinations." Misusing drugs not only is ineffective but also disrupts the vaginal microbiota, causing recurrent inflammation. Today, as a gynecologist, I will explain the "precise treatment plan" for vaginitis once and for all, avoid redundant medication lists, teach you how to treat by type, and cure it without relapse.
Key conclusion first: the core of vaginitis treatment is "first perform routine vaginal discharge testing to classify the type, then use targeted medication." Ms. Li, age 30, had recurrent vaginitis three times and misused drugs each time. Finally, her vaginal discharge test showed "trichomonal vaginitis." She received 1 week of standardized treatment plus partner treatment, and has not had a recurrence in a year. She said, "It turned out I was just messing around before."
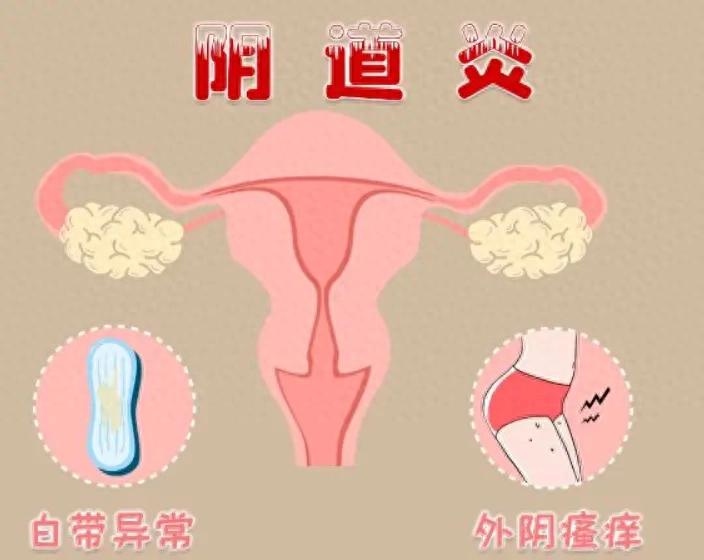
1. First Classify: 4 Common Types of Vaginitis, 30-Second Self-Check (Table Is Clearer)
Types of vaginitis
Typical symptoms (easy to understand at a glance)
Core causes
Key treatment reminders
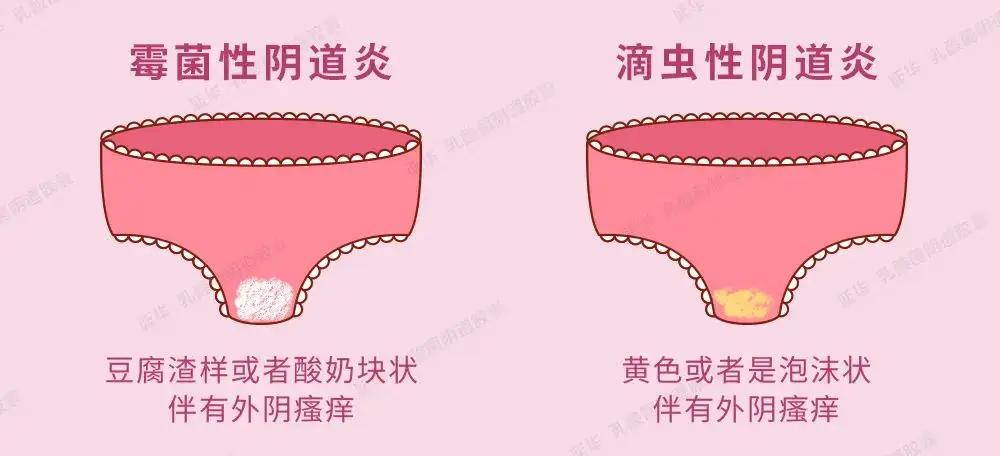
Candidal vaginitis
Leukorrhea resembling tofu dregs / curd-like, vulvar itching to the point of skin breakage, burning pain
Candidal infection (often due to staying up late, high sugar intake, use of antibiotics)
Discontinue antibiotics; antifungal medication required
Trichomonal vaginitis
Yellow-green vaginal discharge, frothy, malodorous, painful during intercourse
Trichomonas infection (primarily sexually transmitted)
Partner must be treated simultaneously, otherwise cross-infection occurs
Bacterial vaginosis
Gray-white, thin leukorrhea with a fishy odor (more pronounced after menstruation)
Vaginal flora imbalance (reduction of beneficial bacteria)
Do not douche with cleansing solutions; lactobacilli need to be replenished
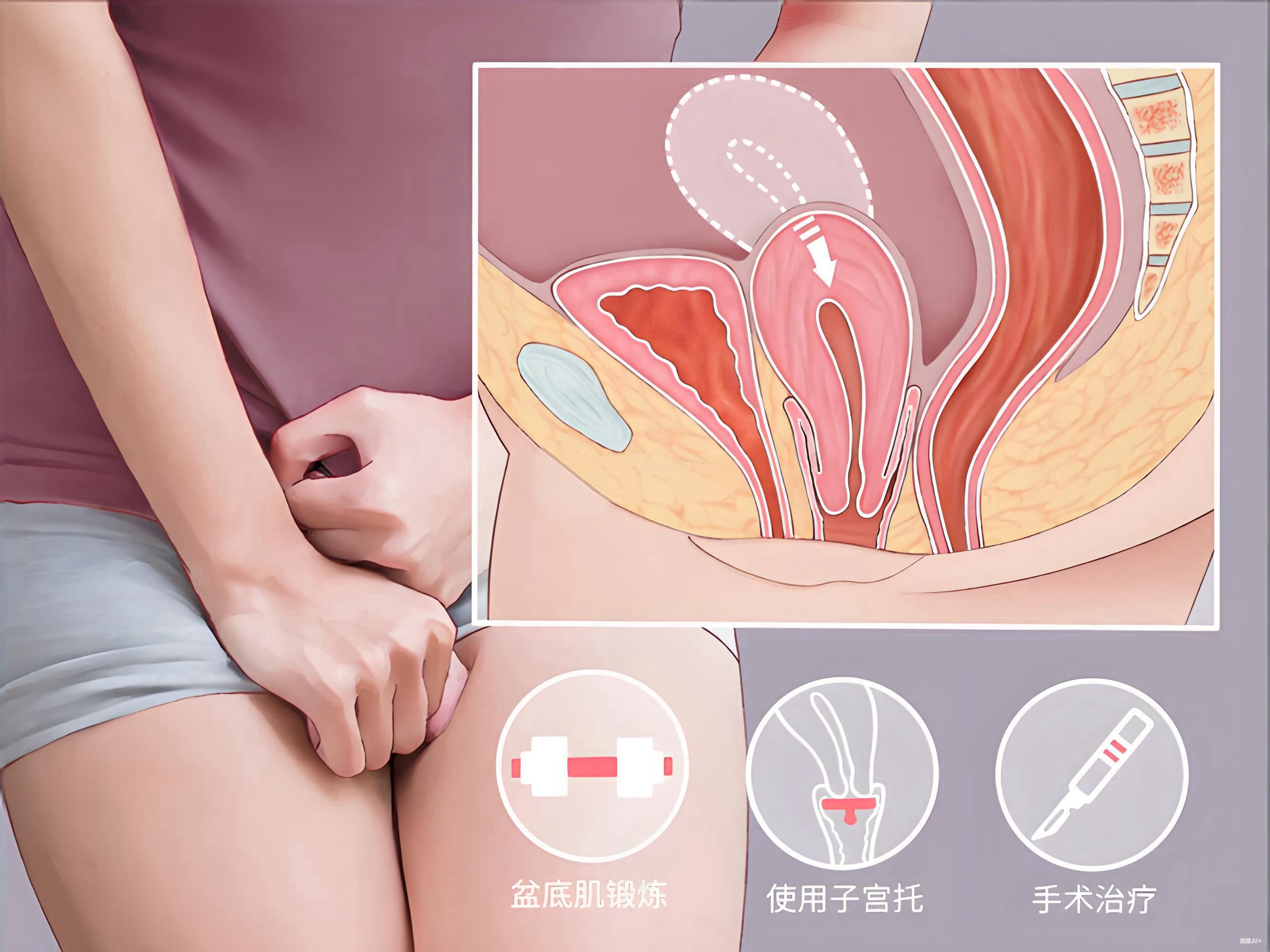
Atrophic vaginitis (senile vaginitis)
Low vaginal discharge, dryness, vulvar itching, dyspareunia
After menopause estrogen declines, mucosa thins
Local estrogen replacement is required to enhance resistance
For example: 25-year-old Xiao Wang had cottage-cheese–like discharge and itching, bought medication for trichomonal vaginitis herself, itching worsened with use, examination showed candidal vaginitis, switched to an antifungal and improved in 3 days — wrong classification, treatment was completely wasted.
2. Precise Treatment Plan: Type-Specific Medication, Get It Right the First Time
1. Candida Vaginitis: Antifungals Are Key, Do Not Use Antibiotics
• Topical agents: clotrimazole suppository / miconazole suppository, 1 tablet daily administered vaginally for 7–14 consecutive days; if there is severe vulvar itching, clotrimazole cream may be applied (avoid the vaginal canal);
• Oral medication: for severe cases take fluconazole as directed by a physician (150 mg, single dose); contraindicated in pregnancy;
• Key point: continue treatment for 3 days after symptoms disappear as consolidation therapy; do not stop medication on your own; during treatment avoid sweets and staying up late to prevent fungal overgrowth.
2. Trichomonal vaginitis: antiprotozoal treatment + partner treated simultaneously, both are indispensable
• Topical agent: metronidazole suppository, 1 tablet daily for 7 consecutive days;
• Oral medication: metronidazole tablets, 400 mg each time, twice daily, for 7 days (take after meals to reduce gastrointestinal irritation);
• Key point: partner must take metronidazole tablets simultaneously (same dose as above); use condoms during treatment, otherwise after you are cured your partner may reinfect you.
3. Bacterial vaginosis: regulate the microbiota, avoid indiscriminate douching
• Topical medication: metronidazole suppository / clindamycin cream, once daily, for 7 days;
• Microbiota regulation: toward the end of treatment use lactobacillus vaginal capsules, one capsule daily for 10 days — replenish beneficial bacteria and rebuild vaginal defenses;
• Key point: Do not irrigate the vagina with washes; wash only the vulva with warm water to avoid disrupting the microbial balance.
4. Atrophic (senile) vaginitis: estrogen replacement + anti-inflammatory treatment, a two-pronged approach
• Topical medications: Estriol cream (local estrogen supplementation to enhance mucosal resistance) + metronidazole suppository (anti-inflammatory), alternate use, continuous for 14 days;
• Oral medications: For severe symptoms, take a small amount of estrogen orally as prescribed (after excluding contraindications to hormones);
• Key point: Eat more soy products (to supplement phytoestrogens), wear 100% cotton underwear, and avoid dryness-related friction.
3. Three Core Treatment Principles: Do These 3 Things to Prevent Recurrence
1. Test before treating; don’t use medications blindly
A routine vaginal discharge test costs only a little over 100 yuan and can accurately determine the type, which is about ten times more reliable than self-diagnosing and medicating. Many people skip testing and directly buy “universal vaginitis medicine,” and the result is worsening condition and development of recurrent vaginitis.
2. Use medication for the full course; don’t stop on your own
This is the number-one culprit of recurrence! For example, vulvovaginal candidiasis requires 7–14 days of treatment; many people stop after 3 days once symptoms ease, but the fungi are not completely eradicated and quickly return. Remember: after symptoms disappear, you must complete the full course of treatment and, if necessary, continue consolidation therapy for 3–5 days.
3. Eliminate precipitating factors to avoid recurrent “irritation” of the inflammation
◦ Hygiene: Wash the vulva daily with warm water, change to pure cotton underwear, scald underwear with boiling water and then sun-dry; after defecation wipe from front to back to avoid contamination of the vagina by anal bacteria;
◦ Lifestyle: Do not stay up late (sleep 7–8 hours per night), eat less sweets and fried foods, avoid long-term use of antibiotics;
◦ Sexual activity: Use condoms during treatment; trichomonal/bacterial vaginosis requires simultaneous treatment of the partner to avoid cross-infection.
4. Three common misconceptions — don’t let treatment go to waste
1. “Douching with a cleansing solution will wash the bacteria away”
Wrong! Douching kills the beneficial bacteria in the vagina, disrupts the microbial balance, and can make vaginitis worse. Washing the vulva with warm water only is sufficient.
2. “If the symptoms disappear, it’s cured and no further medication is needed”
Wrong! Disappearance of symptoms does not mean the pathogen has been completely eradicated. Stopping medication on your own can lead to recurrence of inflammation; you must complete the full course of treatment.
3. “All vaginitis is the same; you can just buy any suppository”
Wrong! Medications for different types of vaginitis are completely opposite. For example, using antibiotics for candidal vaginitis will worsen the condition, and trichomonal vaginitis will lead to recurrent cross-infection if the partner is not treated simultaneously.
5. Special situations: if any of the following occur, seek medical attention promptly
• Vaginitis recurs more than 2 times per year;
• Symptoms have not improved or have worsened after 1 week of medication;
• Accompanied by abdominal pain, fever, or blood-streaked vaginal discharge;
• Pregnant women, patients with diabetes, and postmenopausal women require a physician-designed individualized treatment plan.
Finally, I want to tell you: vaginitis is not a "hard-to-treat disease," but a "disease that is easy to treat incorrectly." As long as you do a "type classification + symptomatic medication + full course treatment + elimination of precipitating factors," the vast majority of people can be cured once and not have a recurrence. Stop self-medicating and indiscriminately douching; spending just over 100 yuan on a routine vaginal discharge test so a doctor can create a precise plan for you will save you money and worry compared with repeated, unnecessary treatments.
If you are currently troubled by vaginitis, don't be anxious—go to the hospital tomorrow for a routine vaginal discharge test and receive targeted treatment—your body deserves to be treated scientifically, not harmed by blind medication!