Is cervical erosion a step toward cervical cancer? 90% are impostors; the real risks are these 2 points
Is cervical erosion a step away from cervical cancer?
"Doctor, I was diagnosed with severe cervical erosion! If I delay treatment, will it turn into cervical cancer?" Every day in clinic I meet women terrified by the two words "erosion" — the term itself carries a "lesion" filter, and private hospitals' scare tactics of "untreated erosion inevitably becomes cancer" have led countless people to spend thousands on "repair surgery" and even suffer psychological trauma. Today, as a gynecologist, I'll lay out the truth at once: cervical erosion has no direct relationship with cervical cancer; 90% is a normal physiological phenomenon. What truly brings you closer to cervical cancer are two "carcinogenic signals" you might be ignoring.
First, a reassurance: Ms. Wang, 42, was diagnosed with severe cervical erosion and was so anxious she had six months of insomnia; her TCT and HPV tests were completely normal, and I told her no treatment was needed—annual follow-up is sufficient. By contrast, Ms. Li, 38, had mild erosion on a checkup, thought it "not serious" and skipped screening; three years later she had postcoital bleeding and was found to be HPV16 positive with a high-grade cervical lesion — this shows that the degree of erosion has nothing whatsoever to do with cancer risk.
1. First, understand: why cervical erosion is not a "precancerous lesion"?
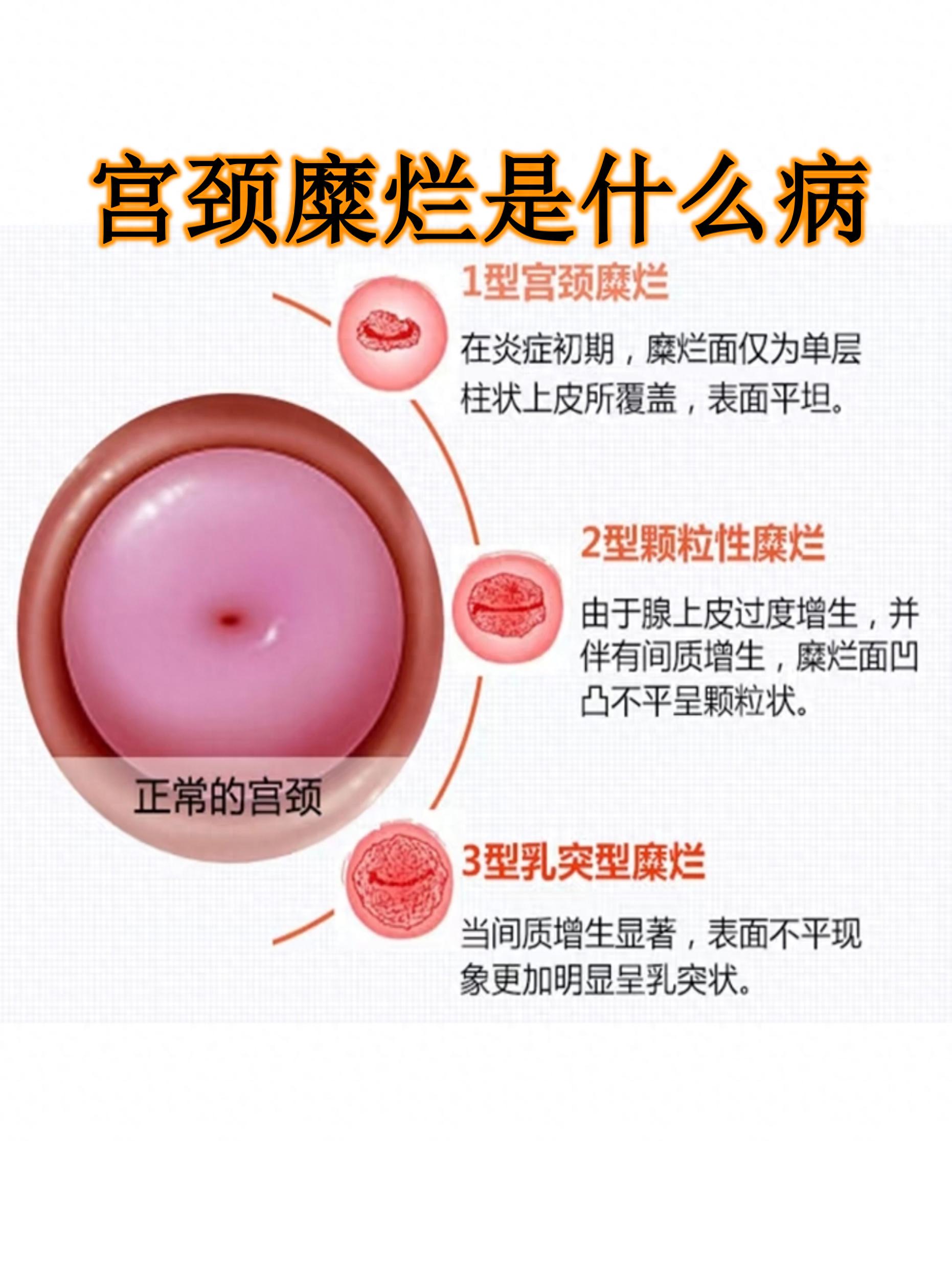
The term "cervical erosion" was removed from medical nomenclature in 2008; its true identity is "cervical columnar epithelial ectopy" and it is essentially a "visual misunderstanding":
The cervix has two "skins": the outer layer (squamous epithelium) is smooth and pink, and the inner layer (columnar epithelium) is thin and red;
When estrogen levels rise (for example in youth, pregnancy, or with use of contraceptives), the inner "red skin" can move outward; to the naked eye this appears as "erosion," but it is actually a normal physiological change of the cervix, like "exposed red mucosa after the lips peel," not true erosion.
Clinical data show: women with cervical ectopy have the same risk of developing cervical cancer as those without ectopy; conversely, many cervical cancer patients have a "smooth" cervix on examination — because early cancer may lack "erosion-like changes" and cannot be detected by gross inspection.
2. The 2 real signals that indicate closer risk for cervical cancer — don’t ignore them!
Cervical erosion is a "disguiser," but these two signs are the "warning lights" for cervical cancer; the appearance of either warrants vigilance:
Persistent infection with high-risk HPV (especially types 16 and 18)
HPV (human papillomavirus) is the "culprit" of cervical cancer; types 16 and 18 account for over 70% of cervical cancers. If these two types are detected positive and the infection persists for more than 2 years, even a smooth-looking cervix confers a tenfold higher cancer risk compared with someone who has erosion but is HPV-negative.
Ms. Zhang, 35, had a smooth cervix but tested HPV18-positive for 3 years; colposcopy revealed a hidden lesion inside the endocervical canal, and timely surgery prevented malignant transformation — this is why the "invisible risk" is more frightening than the "visible erosion."
Abnormal cervical cytology (abnormal TCT report)
TCT testing looks for cellular changes in the cervix; if the report indicates "ASC-H (atypical squamous cells, cannot exclude high-grade lesion)", "LSIL (low-grade lesion)", or "HSIL (high-grade lesion)", it means the cells have already become abnormal and, if not treated, may gradually progress to cancer.
These abnormalities are unrelated to cervical erosion; they can occur even without erosion — for example, 29-year-old Xiao Lin had a smooth cervix but her TCT indicated HSIL, and subsequent biopsy confirmed a high-grade lesion. Fortunately, she underwent timely conization.
3. Practical guide: if cervical erosion is diagnosed, what should be done?
Step 1: Do two tests to distinguish "high vs. low risk"
Whether mild or severe erosion, first test TCT (cytology) + HPV (oncogenic virus):
If both tests are normal and the patient is asymptomatic → no treatment is needed; repeat annual check-up.
If both tests are normal but there is increased vaginal discharge and postcoital bleeding → treat the inflammation (use vaginal suppositories or antibiotics), no need for physical treatments such as laser or cryotherapy;
If HPV positive (especially types 16 or 18) or TCT abnormal → perform colposcopy + biopsy immediately to exclude lesions.
Step 2: Only in these situations should treatment be considered (unrelated to erosion)
Biopsy-confirmed cervical low-/high-grade lesions (the target of treatment is the lesion, not the erosion);
Recurrent inflammation, or leucorrhea/bleeding that severely affects life (microwave treatment can be performed at a qualified hospital to avoid overtreatment).
Step 3: Avoid 3 fatal misconceptions
Misconception 1: "Severe erosion = high cancer risk" → Wrong! The severity of erosion only indicates the extent of "red skin" and is unrelated to pathological lesions;
Misconception 2: "Erosion must be surgically repaired to prevent cancer" → Wrong! Physiological erosion does not require repair; surgery can damage the cervical mucosa and impair its defenses;
Misconception 3: "No erosion means no need for screening" → Wrong! Many cervical cancer patients have a smooth cervix. Sexually active women aged 21 and over should have a TCT once a year, and after 30 add HPV testing; this is the key to cancer prevention.
4. Final summary: remember 3 sentences to stay away from anxiety and risk
Cervical erosion is a "physiological misunderstanding," not a disease, no need to fear;
The "culprit" of cervical cancer is persistent infection with high-risk HPV + cellular abnormalities, unrelated to erosion;
Preventing cervical cancer relies on "screening," not "treating erosion"; regular TCT + HPV testing is the reliable approach.
As a gynecologist, I have seen too many women panic over "cervical erosion," and I have also seen cases where screening was neglected and treatment delayed. The key to health is actually simple: don't be frightened by the name, and don't ignore screening. If you currently have a "cervical erosion" report in hand, don't panic—first get TCT and HPV testing— in most cases you will receive the reassuring conclusion "no treatment needed," and that is the most responsible choice you can make for yourself!