Orthopedic Surgeons Use 7 Mahjong Terms to Help You Understand the Root Cause and Symptoms of Knee Osteoarthritis
A Scientific Approach to Joint Aging
Knee osteoarthritis is the "number one joint killer" affecting hundreds of millions of middle-aged and elderly people worldwide. Although this age-related joint disease cannot be cured, we can definitely keep our knees "strong in old age" through scientific methods!

Many friends might be familiar with the "Seven Pairs" hand in mahjong. Today, I will use the "Seven Small Pairs" mnemonic to summarize seven easy-to-understand keywords, helping you master all the essentials for treating knee osteoarthritis!
I. Root Cause Strategy: Slowing Disease Progression from the Source
01 First Pair: Reduce – "Unload" the Knees
Your knees are like a "human crane." For every 1 kg increase in body weight, the pressure on your knees while walking surges by 3 kg! Studies confirm that the incidence of osteoarthritis in obese patients is 12%–43%. Statistical results show that for every 4.5 kg weight gain, the incidence of knee osteoarthritis can increase by 40%. For every pound (approximately 0.45 kg) of excess weight, the load on the knee joint surface cartilage increases 3 to 6 times.
One study confirmed that with an average weight loss of 5 kg in women, the risk of knee osteoarthritis decreased by 50%. This suggests that weight loss can reduce the risk of knee osteoarthritis progression in obese patients. However, it's important to note that weight loss should be gradual; excessive dieting may lead to muscle loss, which can actually harm joint stability.
Action Guide:
1. For those overweight: Aim for a 5%-10% weight loss through dietary control + low-impact exercises like swimming and cycling.
2. For those with normal weight: Avoid unnecessary weight loss; maintaining muscle mass is more important.

02 Second Pair: Train – "Reinforce" the Knees
The muscles surrounding the knee joint are natural "knee braces." The quadriceps at the front of the thigh, the hamstrings at the back, and the gluteal muscles act like "steel bars," while the core muscles serve as the "foundation," collectively maintaining joint stability. Targeted muscle training can enhance the dynamic stability of the knee joint.
Recommended Exercises:
1. Straight Leg Raise (External Rotation):

(1) Lie flat on your back with legs straight, feet together, and toes turned outward.
(2) First flex your foot, then straighten the knee joint, slowly raise the leg to about a 30-degree angle, hold for a few seconds; slowly lower it and repeat with the other leg.
(3) Frequency: 15 raises per leg constitutes one set; aim for 3 sets per day.
2. Wall Sit:

(1) Stand with your back against a wall, feet shoulder-width apart, slowly squat down (at most) until your thighs are parallel to the ground, hold for 30 seconds (can be extended based on individual capability) to activate the front thigh muscles.
(2) Individuals experiencing pain in the front of the knee when climbing stairs or squatting should avoid this exercise.
3. Glute Bridge:

(1) Lie on your back with knees bent slightly wider than shoulder-width, heels on the floor. Engage your glutes to lift your hips until your thighs and torso form a straight line.
(2) Keep your upper back supported on the ground as you lift your hips; when lowering, let your lower back touch the ground but keep your hips slightly elevated. Exhale as you lift your hips, inhale as you lower them. Feel a strong contraction and squeeze in your glutes at the top, hold for 2 to 4 seconds, then return to the starting position.
(3) 15-20 repetitions per set, 3-5 sets.
4. Clamshell (with Resistance Band):

(1) Lie on your side on a yoga mat with knees bent at about 90 degrees, heels and back aligned. Place your top hand on the floor in front of your chest for support, and cushion your head with your bottom hand to maintain a neutral neck position. Place a resistance band (15-20 lbs resistance) just above both knees.
(2) Engage your glute muscles to open the top leg upward to its maximum range, keeping your core tight and body stable. Then lower the leg back to the starting position where the knees are close but not touching.
(3) Exhale as you open, inhale as you lower. Perform the movement slowly, not too fast. Do 10-15 repetitions per set, 3-5 sets per day, resting 30-60 seconds between sets. Activating the gluteus medius can reduce the risk of knee arthritis by 62%.
Note: Apply ice for 10 minutes after each training session to avoid mistaking muscle soreness for joint pain.
II. Symptomatic Management: Acute Phase Care
03 Third Pair: Rest – Give Your Knees a "Break"
When your knees hurt, don't push through! Just like resting when you have a fever, knees also need to "recharge their batteries." Short-term rest is not "being lazy"; it's to allow joint inflammation to subside faster.
Acute pain phase: Reduce walking or weight-bearing activities; use crutches or a walker if necessary. Avoid the misconception of "the more it hurts, the more you should exercise." Short-term rest (1-2 weeks) can actually extend joint lifespan.
Note: Do not remain immobile for long periods because you think your knee joint is inflamed, aging, or you fear wear and tear, believing it protects the joint. In reality, prolonged immobilization leads to muscle atrophy, making the knee joint more prone to "failure"! Those who sit for long periods should get up and move for 5 minutes every hour to avoid joint stiffness.

04 Fourth Pair: Treat – "Put Out the Fire" in Your Knees
Inflammation is the "fuse" for pain. Treatment should be approached in layers:
1. Topical First: Prefer topical NSAID gels (e.g., Flurbiprofen). Those with allergies can use gel patches. For medicated plasters: Do not use continuously for more than 2 weeks, change the application site daily, with a 4-6 hour interval. Note if traditional Chinese medicine plasters require application every other day.
2. Oral Medication with Caution: Etoricoxib, Diclofenac Sodium, Ibuprofen, Celecoxib (contraindicated in sulfa allergy), etc. For short-term use: not exceeding one week for acute pain; generally 3-4 weeks for chronic pain, maximum not exceeding 3 months (rarely); and do not combine two medications.
3. Physical Therapy: Ultrasound, shockwave therapy, etc., can improve local circulation and should be performed under the guidance of a doctor or physical therapist.
4. Caution: Be wary of "miracle drugs" from unregulated clinics: they are mostly corticosteroid-based. Continuous use can lead to serious risks like osteoporosis and femoral head necrosis.
Inflammation is the "culprit" of pain, and treatment must be step-by-step. Start with topical medication for "local firefighting." If the pain is severe, use oral medication for "full suppression," but never believe in "miracle drugs"—overuse of steroids can harm the body! Also, don't believe in knee supplements; they are mostly a waste of money.

III. Surgical Intervention: Precise Repair and Reconstruction
When conservative treatments are ineffective, surgical intervention should be considered, which can be divided into three stages:
05 Fifth Pair: Repair – "Realign" the Knees
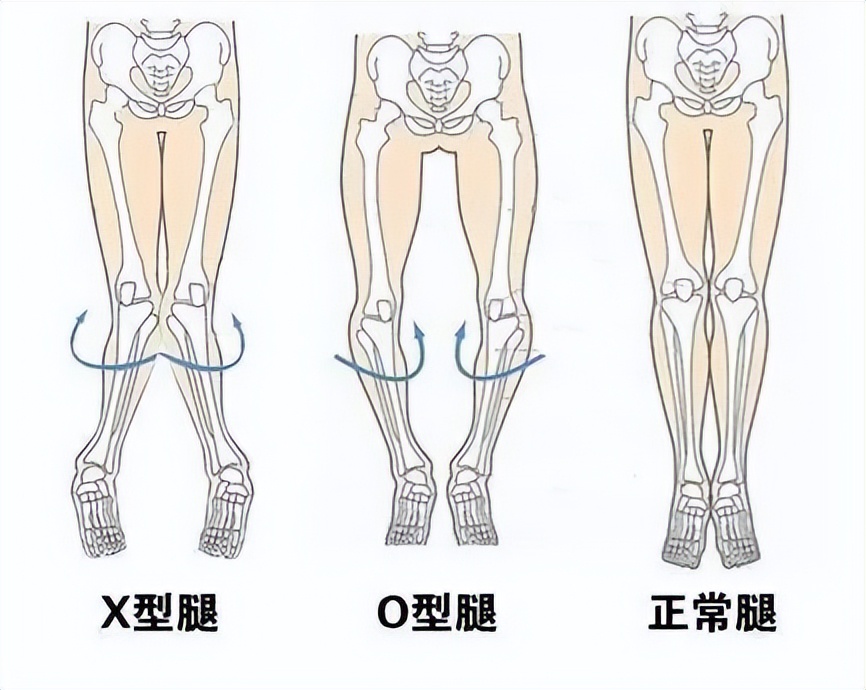
For patients with bowlegs (O-shaped legs) or knock-knees (X-shaped legs) whose cartilage condition is still acceptable, high tibial osteotomy can adjust the lower limb alignment, shifting the weight-bearing area to relatively healthier cartilage. This is like "getting a wheel alignment for a misaligned car," allowing the knee to bear weight more evenly with less wear. The vast majority of patients can delay arthritis progression by 5-10 years post-surgery.
Suitable Candidates:
1. Relatively young patients whose joint cartilage is not completely worn.
2. X-rays show joint space is present, but lower limb alignment deviation >5°.
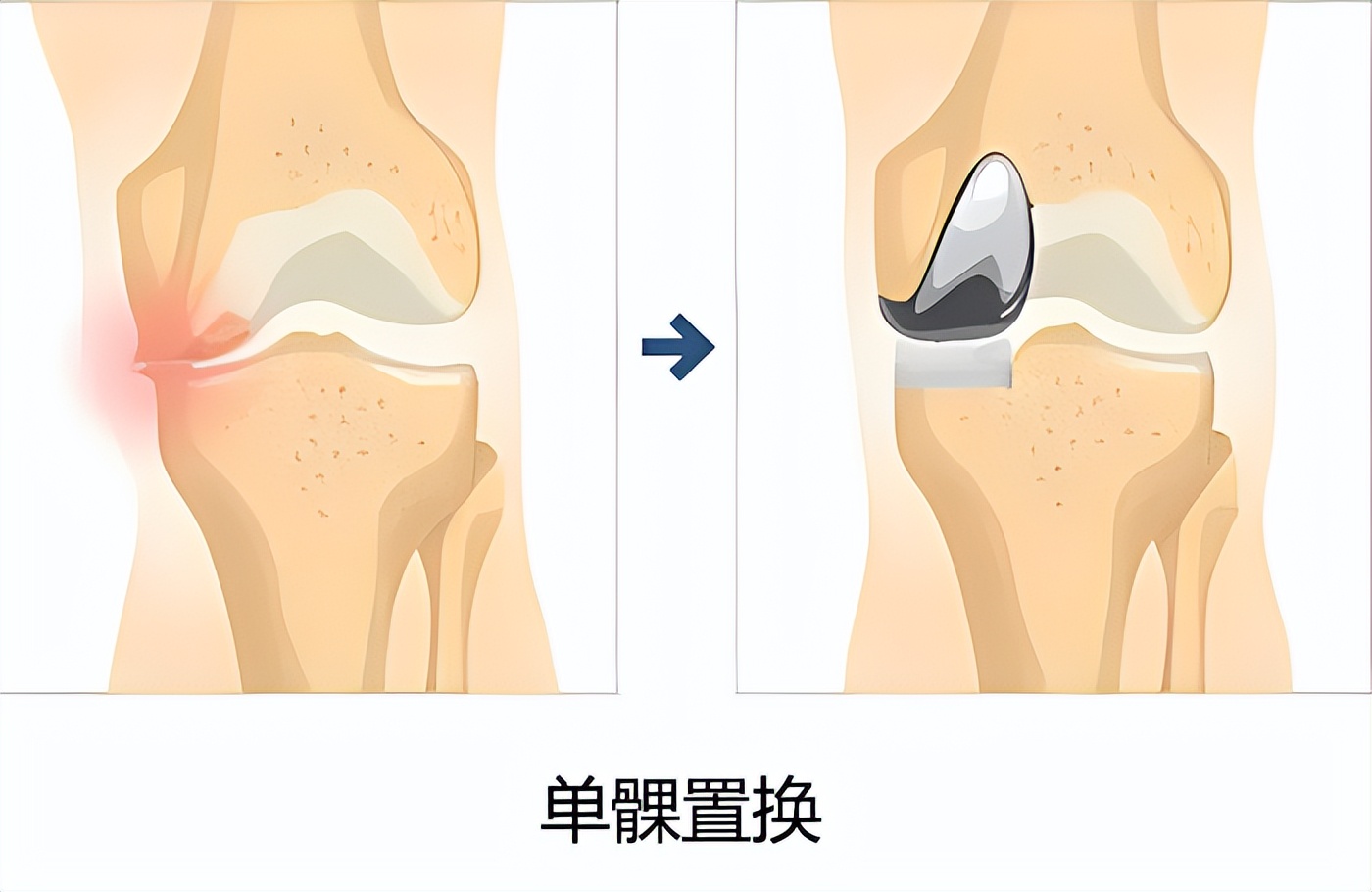
06 Sixth Pair: Patch – "Patch Up" the Knees
For patients with single-compartment knee disease, only the worn cartilage surface is replaced, preserving the cruciate ligaments and meniscus. This is like "patching a worn tire"—only the damaged part is replaced, and healthy tissue is retained. Postoperative recovery is faster, and the feeling is more natural, making it particularly suitable for friends with single-compartment knee disease.
Advantages:
1. Postoperative proprioception retention rate reaches 90%, and recovery time is only one-third that of total knee replacement.
2. Suitable for patients with single-compartment disease (e.g., only medial cartilage wear).
07 Seventh Pair: Replace – Give Your Knees a "New Life"
When knee osteoarthritis progresses to the point where the joint cartilage has completely disappeared, many friends who have worked hard all their lives and are still physically capable in their sixties or seventies find their knees worn out, leading to a drastic decline in quality of life. At this stage, there's no need to endure any longer. Total knee replacement surgery is your only "lifeline."
Suitable Candidates:
1. Imaging shows the joint space is very narrow or even absent, having progressed to the "bone-on-bone" stage.
2. Knee pain symptoms are severe, daily activities are significantly limited, the patient feels considerable distress, and quality of life is noticeably affected.

Long-term Strategy: "Peaceful Coexistence" with Arthritis
Understand the "Seven Small Pairs" mnemonic and adopt the concept of "living with the disease." Please remember: The treatment goal is not "reversing aging," but through scientific management, maintaining the joint's optimal functional state during the aging process. As orthopedic experts say: "Rather than seeking a cure, learn to dance gracefully with arthritis."