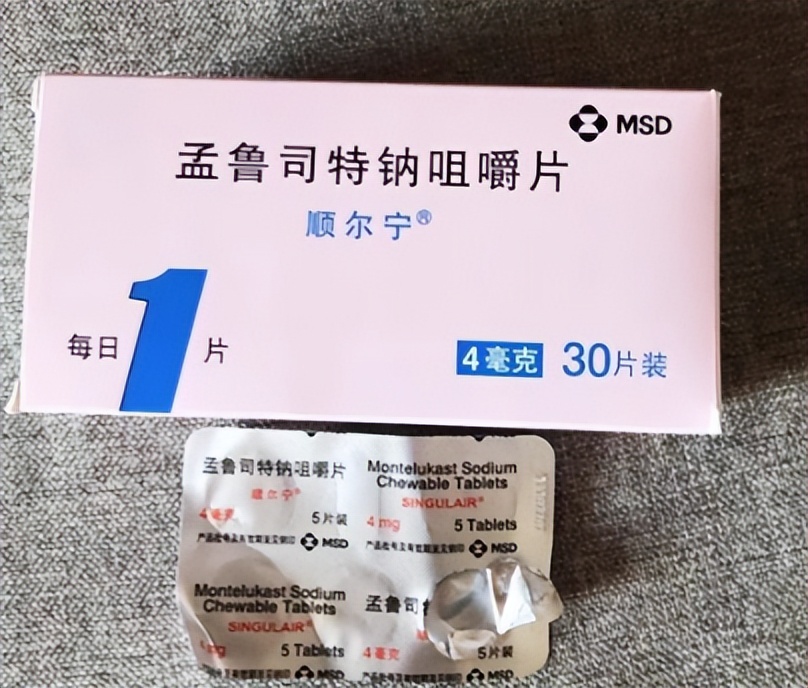
Worried about the side effects of montelukast sodium? Experts teach you how to safely switch medications
If you or your child are using montelukast sodium to treat asthma or allergic rhinitis, you may have recently noticed a warning: this medication may carry risks of neuropsychiatric side effects affecting mood, sleep, and related nervous-system functions.
This has worried many families. Don’t panic — if a medication change is needed because of side effects, there are many long-established, safe, and effective clinical alternatives. This article will clearly outline them to help you be better prepared when communicating with your doctor.

Part 1: Why should we pay attention to montelukast sodium?
。
Montelukast sodium is an effective anti-inflammatory and anti-allergic drug. But one relatively special risk is that a very small number of people (especially children) may experience changes in mood or behavior after use.
Possible manifestations include: insomnia, anxiety, irritability, nightmares, and even more severe aggression or depressive symptoms.
Although the incidence is low, once it occurs it has a great impact on the patient and family. Therefore, understanding alternative options and being informed is very necessary.
Part Two: What alternative options are there for asthma patients?
Asthma treatment is like a combination of punches; montelukast sodium is just one of them and can be completely replaced by other, safer "punches."
Top choice ace: inhaled corticosteroids (such as budesonide, fluticasone)
Why are they the first choice? These are the most central and effective drugs for controlling airway inflammation in asthma. They act directly on the lungs, like a precise fire extinguisher for inflamed lungs, with minimal systemic absorption.
:
Greatest advantage: It hardly causes the neuropsychiatric side effects associated with montelukast sodium; its safety record is excellent, and it is the preferred first-line maintenance therapy recommended by domestic and international guidelines.
Tip: Use the correct inhalation technique and rinse your mouth well after use to effectively prevent local issues such as oral fungal infections.
Other important options:
Quick-relief medication (rescue drug): such as salbutamol inhaler. This is the "emergency hero"; when asthma attacks suddenly occur it can rapidly dilate the airways, but it should not be relied on daily to control the condition.
Other types of controller medications:
Long-acting bronchodilators: should be used in combination with inhaled corticosteroids, working synergistically.
Anticholinergic agents: such as tiotropium bromide, which are very effective for certain types of asthma (e.g., concomitant COPD).
Another leukotriene modulator: such as pranlukast, with a similar mechanism of action but a lower risk of psychiatric side effects, and is also an option.
"Ultimate weapon" — biologics: such as omalizumab, which target severe, refractory asthma with pinpoint precision, but require injections, are expensive, and have strict indications.
Part Three: For patients with allergic rhinitis, switching medications is easier!
For allergic rhinitis, there are many alternatives to montelukast sodium, and they often work better.
First-line oral medications: new-generation antihistamines (such as cetirizine, loratadine, levocetirizine)
Core advantages: very safe, almost never causes drowsiness, and no concerns about psychiatric side effects. Acts quickly and is clearly effective for symptoms such as sneezing, runny nose, and itchy nose.
Small fact: Today’s "new-generation" drugs have greatly improved on the old-generation medications (such as chlorpheniramine), which caused drowsiness after use.
Topical first-line: intranasal steroid sprays (such as mometasone furoate, fluticasone propionate)
Why especially recommended? These are among the most effective drugs for treating nasal congestion. They are sprayed directly into the nasal cavity, act locally, are virtually not absorbed systemically, and have very high safety; they can be used long-term in both children and adults. For moderate to severe rhinitis, their effect is usually superior to montelukast sodium.
A gentle option: sodium cromoglicate nasal drops
Very suitable for patients with mild symptoms or for parents who are very concerned about steroids (although intranasal steroids are actually very safe). Their side effects are minimal, but they act more slowly and are usually used for prevention.
Part Four: Special Care for Special Populations
Medication for children:
Childhood asthma: Inhaled steroids (such as budesonide) are internationally recognized as the first-line and safe choice; use under physician guidance, with benefits far outweighing risks.
Childhood rhinitis: New-generation antihistamines (such as cetirizine syrup) or intranasal steroid sprays are preferred.
Pregnant and breastfeeding mothers:
Use of medication requires extreme caution. Budesonide inhalers or nasal sprays are generally relatively safe options. A key step: be sure to consult your doctor and make decisions together.
Remember the most important point: never stop or switch medications on your own!
Sudden discontinuation of montelukast sodium may lead to symptom rebound. The correct approach is: schedule an appointment with your doctor or specialist. Communicate your concerns openly and describe in detail any discomfort you or your child are experiencing. Discuss with the doctor to develop a safer, individualized treatment plan that best suits your condition.
In summary: whether it’s asthma or allergic rhinitis, there are many excellent alternatives to montelukast sodium. Inhaled/nasal steroids and the new generation of oral antihistamines are the two main safe and effective forces. You can entirely have your condition controlled while avoiding unnecessary risk of side effects.