The Diagnosis of Chronic Prostatitis Must Satisfy Two Levels
Chronic prostatitis is a common disease in men; only with an accurate diagnosis can treatment be more effective. The diagnosis of chronic prostatitis must include the following two levels:
Level One: Classification Diagnosis
Strictly speaking, prostatitis is a collective term for a group of diseases, and the classification and diagnosis of prostatitis provide the basis for standardized and accurate clinical treatment. Currently, the classification of prostatitis primarily utilizes the National Institutes of Health (NIH) criteria, which are divided into four types: Type I is acute bacterial prostatitis; Type II is chronic bacterial prostatitis; Type III is chronic non-bacterial prostatitis/chronic pelvic pain syndrome (CPPS); and Type IV is asymptomatic inflammatory prostatitis. Therefore, chronic prostatitis mainly refers to the latter three types. Through this classification, it can be clarified which types of prostatitis require treatment and which do not, as well as which require antibiotics and which can be managed without them. The basis for classification diagnosis primarily includes clinical symptoms, routine examination of prostatic fluid, and bacterial culture of prostatic fluid.
Level Two: Comprehensive Diagnosis
Since chronic prostatitis belongs to a group of multi-symptomatic diseases, diagnosis through comprehensive analysis is crucial.
1. Clinical Symptoms
Chronic prostatitis often presents with symptoms such as urinary discomfort, pain, sexual dysfunction, general malaise, and psychological symptoms, which can be used to roughly assess the condition. The primary basis for diagnosing chronic prostatitis is the symptoms, and evaluating the effectiveness of treatment also relies mainly on the degree of symptomatic improvement.

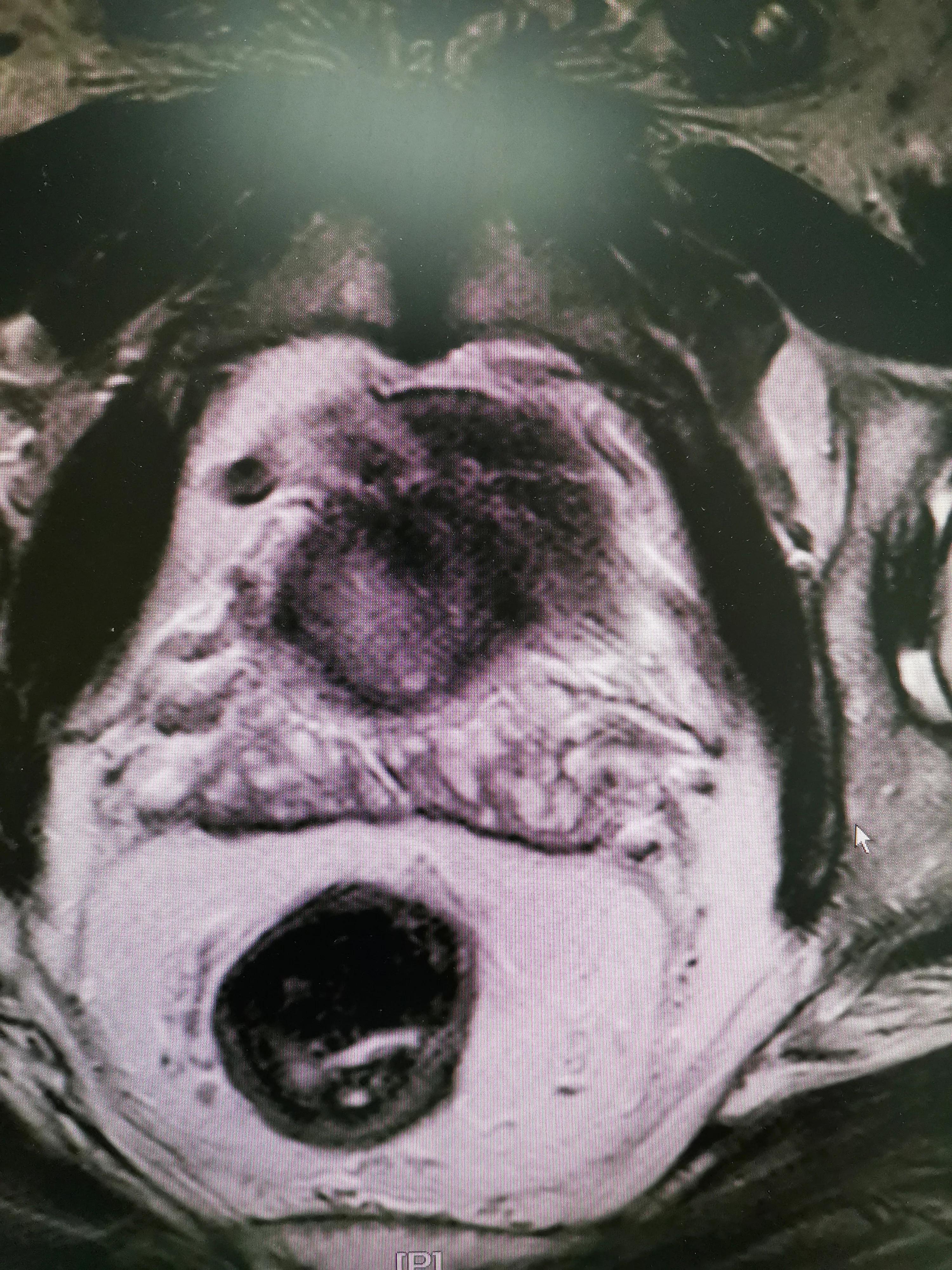
2. Digital Rectal Examination (DRE)
Through a digital rectal exam, one can determine the size, texture, tenderness, and presence of nodules in the prostate. This is particularly important for differentiating it from other prostate diseases, such as benign prostatic hyperplasia (BPH) and prostate cancer.
3. Prostatic Fluid Examination
Prostate fluid examination primarily includes routine prostate fluid analysis and bacterial culture. If the routine analysis shows a white blood cell count above 10/HP and a decrease in lecithin bodies, chronic prostatitis can be considered. If the bacterial culture of the prostate fluid is positive, a diagnosis of bacterial prostatitis can be made.
4. Urinalysis
The primary purpose of a urinalysis is to check for an elevated white blood cell count, thereby ruling out the possibility of a urinary tract infection.
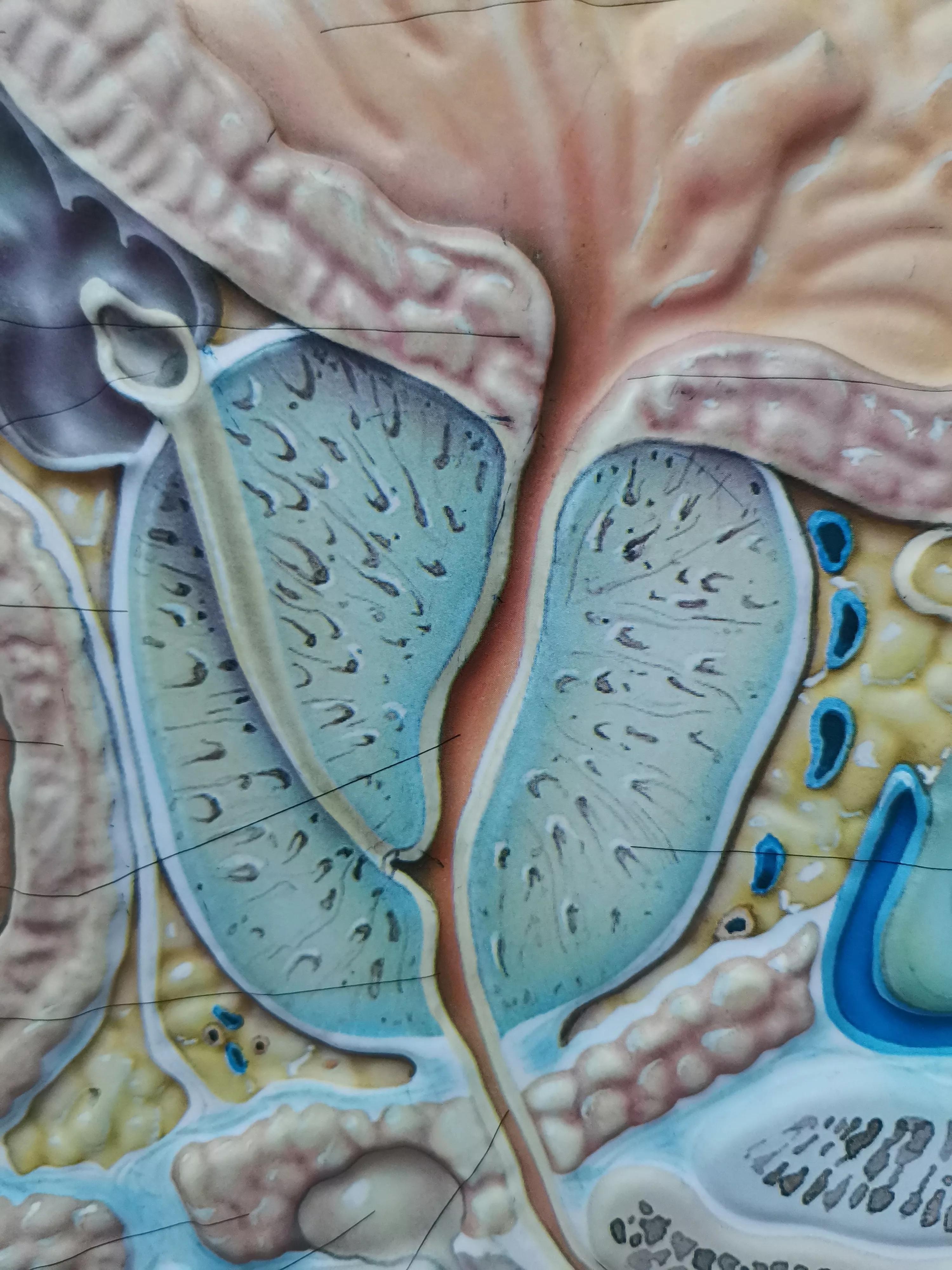
5. Color Ultrasound Examination
Color Doppler ultrasound of the prostate (especially transrectal ultrasound) allows for an accurate assessment of the prostate's size and structure, determines the presence of inflammatory changes, and identifies any masses, nodules, or calcifications.
6. Other examinations
If other diseases need to be ruled out, additional tests are required, such as uroflowmetry and urodynamic studies (used to determine the presence of bladder dysfunction or bladder outlet obstruction) and cystoscopy (to examine the structure of the entire urethra and bladder and identify issues such as prostatic hyperplasia).
Through a comprehensive analysis of typical symptoms and the aforementioned tests, and by ruling out other conditions, a definitive diagnosis can essentially be established!