What is the connection between prostatitis, seminal vesiculitis, and epididymitis?
The three major inflammatory diseases of the male reproductive system are prostatitis, seminal vesiculitis, and epididymitis. So, what exactly are the connections and differences between these three diseases? Let's discuss them briefly below!
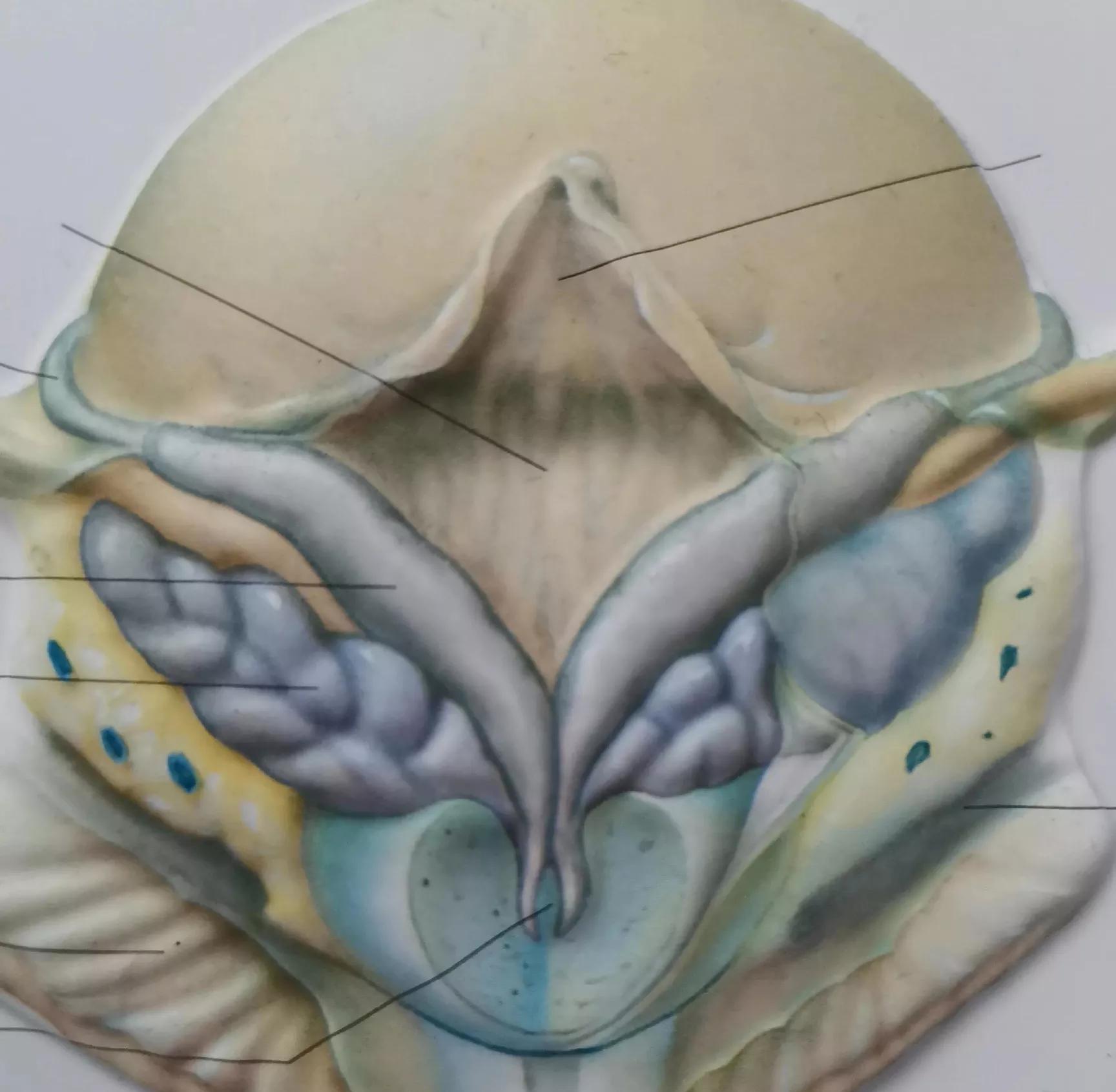
First, let's understand some anatomy of the male reproductive system. The male reproductive system is divided into reproductive glands, accessory sex glands, and the reproductive tract. The reproductive glands primarily refer to the testes and the epididymis, which are the sites where sperm are produced and matured; specifically, the epididymis is where sperm mature and also serves as part of the sperm transport channel, with the distal tail of the epididymis connecting to the vas deferens. The seminal vesicles are accessory sex glands in men, responsible for secreting and producing seminal vesicle fluid and providing a temporary storage site for sperm; their distal ends are continuous with the vas deferens. The prostate is also a male accessory sex gland and is the largest one; it is the site where prostatic fluid is secreted and produced. It also forms part of the male urethra, known as the prostatic urethra, and is located closely to the seminal vesicles. The proximal end of the prostate is continuous with the bladder outlet, while the distal end is continuous with the rest of the urethra.
As can be seen from the anatomical features described above, the epididymis, seminal vesicles, and prostate are all part of the male reproductive system and share intricate connections.
Prostatitis is an inflammatory disease of the prostate. The source of inflammation may originate from the bladder or distal urethra, or it may stem from the reproductive tract—specifically the seminal vesicles (as the prostate and seminal vesicles are located in close proximity). Conditions such as cystitis, urethritis, or seminal vesiculitis may spread to the prostate, triggering prostatic inflammation.
In clinical practice, patients with hematospermia (blood in the semen) are frequently encountered and often found to have concurrent prostatitis. This may occur because prostatitis has spread to the seminal vesicles, or seminal vesiculitis has spread to the prostate. It is also significantly related to factors such as an overly narrow ejaculatory duct, tumor compression in the ejaculatory duct area, or seminal vesicle stones.
Most cases of epididymitis are caused by retrograde infection. In other words, the pathogenic microorganisms in epididymitis often originate from infections in the distal sperm duct or accessory sex glands that eventually spread to the epididymis. The most common underlying conditions are prostatitis and seminal vesiculitis. Certain specific infections can also cause retrograde infection; for example, tuberculosis of the bladder or urethra and seminal vesicle tuberculosis can lead to retrograde infection, resulting in tuberculosis of the vas deferens and epididymis.
The symptoms produced by these three types of inflammation are sometimes very similar. For example, both prostatitis and seminal vesiculitis can cause a heavy, swelling pain around the perineum, while epididymitis itself causes localized swelling and pain. During acute flare-ups of any of these three conditions, a routine urinalysis may show an elevated white blood cell count. All three inflammatory diseases have the potential to decrease the quality of a man's semen and sperm, thereby affecting normal reproductive function.

When treating prostatitis, seminal vesiculitis, and epididymitis, the antibiotics selected are often those effective against all three conditions simultaneously, such as quinolones (e.g., levofloxacin) and macrolides (e.g., roxithromycin, clarithromycin, azithromycin). Throughout the treatment process for these three diseases, it is crucial to emphasize avoiding prolonged sitting and excessive sexual activity; the diet should be light, and alcohol consumption must be avoided.